Understanding Neurological Disorders
To gain a comprehensive understanding of neurological disorders, it is essential to delve into the nuances of neurological conditions and emphasize the significance of early diagnosis. Neurological disorders can encompass a wide range of conditions that affect the brain, spinal cord, and the intricate network of nerves throughout the body.
Overview of Neurological Conditions
Neurological conditions span a spectrum of disorders that impact the brain, spinal cord, and nerves, influencing various aspects of neurological function. These conditions can manifest in diverse symptoms, ranging from cognitive impairments to physical limitations. Diagnosis for neurological conditions involves a battery of tests such as CT scans, MRI, EEGs, and PET scans, administered by radiologists or technologists, to evaluate conditions like brain injury, tumors, epilepsy, or stroke (Johns Hopkins Medicine).
The realm of neurological disorders includes a plethora of specific conditions, such as Acute Spinal Cord Injury, Ataxia, Brain Tumors, Hydrocephalus, Meningitis, Muscular Dystrophy, Cluster Headaches, Tension Headaches, Migraine Headaches, and Cerebral Aneurysm (Johns Hopkins Medicine). Each condition presents unique challenges and requires tailored approaches to diagnosis and treatment.
Importance of Early Diagnosis
Early diagnosis plays a pivotal role in the management and treatment of neurological disorders. Timely identification of neurological conditions allows for prompt intervention and appropriate treatment strategies to mitigate potential complications and improve outcomes. Whether it is detecting signs of stroke, identifying indicators of migraines, or diagnosing brain tumors, early diagnosis is instrumental in providing targeted care and support to individuals grappling with neurological disorders.
By recognizing the symptoms early on and harnessing the advancements in diagnostic modalities, healthcare providers can offer timely interventions and personalized treatment plans for individuals affected by neurological conditions. Additionally, early diagnosis can enhance the effectiveness of therapeutic interventions and pave the way for better prognoses for patients navigating the complexities of neurological disorders.
Understanding the landscape of neurological disorders and the pivotal role of early diagnosis is crucial in promoting awareness, fostering research, and enhancing the quality of care for individuals grappling with these intricate conditions. Stay informed, seek professional guidance, and prioritize early detection to navigate the realm of neurological disorders with diligence and compassion.
Common Neurological Disorders
Among the myriad of neurological disorders and treatments, several are prevalent in today’s society. Understanding the causes and appropriate management strategies for disorders like ALS (Amyotrophic Lateral Sclerosis), an aneurysm, and Alzheimer’s disease is crucial for both patients and their caregivers.
ALS: Causes and Treatments
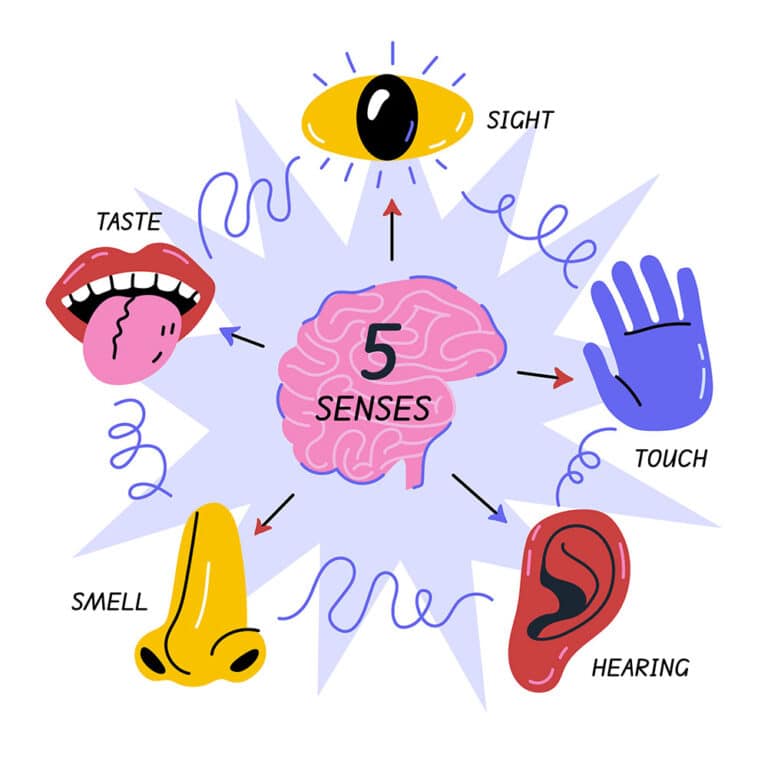
ALS, commonly known as Lou Gehrig’s disease, is a progressive neurological disorder that primarily affects motor neurons, leading to muscle weakness, paralysis, and ultimately impacting speaking, swallowing, and breathing functions (Health First). While ALS does not typically affect sensory or cognitive functions, it significantly impairs physical abilities.
Treatment for ALS focuses on symptom management and improving the quality of life for patients. Medications can be prescribed by healthcare professionals to help alleviate symptoms and slow down the progression of the disease. Additionally, therapies such as physical and occupational therapy play a crucial role in maintaining mobility and independence for individuals with ALS.
Aneurysm: Surgical Options
An aneurysm refers to an abnormal bulging or ballooning of a weakened blood vessel in the brain. The condition poses a significant risk as the aneurysm can rupture, leading to potentially fatal consequences such as severe disability, cognitive impairment, or even death (Health First).
The treatment of aneurysms involves a combination of traditional medical approaches and advanced surgical techniques. Depending on the size, location, and condition of the aneurysm, treatment options may include surgical clipping, endovascular coiling, or endovascular embolization. These procedures aim to prevent the rupture of the aneurysm and alleviate the pressure on the surrounding brain tissue, thereby reducing the risk of severe complications.
Alzheimer’s Disease Management
Alzheimer’s disease is the most common cause of dementia, characterized by the progressive deterioration of memory, thinking, and behavior. While there is currently no cure for Alzheimer’s, various medications and management strategies are available to help alleviate symptoms and improve quality of life for individuals living with the disease (Health First).
Medications prescribed for Alzheimer’s disease focus on managing cognitive symptoms such as memory loss, confusion, and communication difficulties. Additionally, lifestyle modifications including cognitive stimulation activities, physical exercise, and a healthy diet can help slow down the progression of the disease and improve overall cognitive function.
By understanding the causes and treatment options for common neurological disorders like ALS, aneurysms, and Alzheimer’s disease, individuals can make informed decisions regarding their healthcare and seek appropriate support and resources for managing these conditions.
Managing Neurological Conditions
When it comes to managing neurological conditions, tailored treatment approaches and care strategies play a vital role in improving the quality of life for individuals affected by these disorders. In this section, we will explore the treatment approaches for epilepsy, care strategies for Parkinson’s disease, and the symptoms and support available for dementia patients.
Epilepsy Treatment Approaches
Epilepsy, a central nervous system disorder characterized by seizures or unusual behavior, can be effectively managed through various treatment approaches. According to Health First, epilepsy is typically treated with prescription medication. Antiepileptic drugs are commonly prescribed to help control and prevent seizures. It’s essential for individuals with epilepsy to adhere to their medication regimen as prescribed by their healthcare provider to minimize the frequency and intensity of seizures.
In cases where medications do not provide adequate seizure control, alternative treatment options like surgery or other medical interventions may be considered. Surgical procedures such as brain surgery or nerve stimulation can be beneficial for individuals with drug-resistant epilepsy. These interventions aim to reduce or eliminate seizure activity by targeting specific areas of the brain responsible for the seizures.
Parkinson’s Disease Care Strategies
Parkinson’s disease, a progressive nervous system disorder that affects movement and speech, requires comprehensive care strategies to address the multifaceted symptoms associated with the condition. While there is currently no cure for Parkinson’s disease, medications can help manage motor symptoms such as tremors, stiffness, and slowness of movement.
As highlighted by Health First, individuals with Parkinson’s disease may benefit from therapies like aerobic exercise, physical therapy, stretching exercises, and speech therapy. These interventions are aimed at improving mobility, balance, and speech abilities, thereby enhancing the overall quality of life for patients with Parkinson’s disease.
In advanced stages of the disease, surgical options like deep brain stimulation surgery may be recommended. This procedure involves implanting electrodes in specific areas of the brain to help regulate abnormal brain activity and alleviate motor symptoms.
Dementia Symptoms and Support
Dementia, an umbrella term for brain diseases like Alzheimer’s disease, presents unique challenges due to its progressive nature and impact on cognitive function. As highlighted by MedStar Health, seeking medical help for dementia symptoms is essential for timely diagnosis and appropriate management.
While there is no cure for dementia, medications can help manage memory symptoms and cognitive changes associated with the condition. Additionally, individuals with dementia may benefit from non-pharmacological interventions such as cognitive therapies, occupational therapy, and engagement in social activities. Support groups for both patients and caregivers can provide invaluable emotional support and practical guidance in navigating the complexities of dementia care.
By addressing the unique needs of individuals with epilepsy, Parkinson’s disease, and dementia through personalized treatment approaches and care strategies, healthcare providers can significantly impact the lives of those affected by these neurological conditions. Collaboration between patients, caregivers, and healthcare professionals is essential in ensuring comprehensive management and support for individuals living with neurological disorders.
Promising Advances in Neurology
Keeping up with the latest advancements in the field of neurology is essential for understanding the cutting-edge treatments and therapies available for various neurological disorders. In this section, we will delve into three promising advances: gene therapy prospects, brain-computer interfaces, and virtual reality therapy benefits.
Gene Therapy Prospects
Gene therapy is anticipated to revolutionize the treatment of neurological disorders, including Huntington’s disease, Parkinson’s disease, ALS, and Alzheimer’s disease, by modifying genes to prevent or reverse their effects (Foothills Neurology). In 2024, significant progress is expected in the field of gene therapy, offering new hope for individuals suffering from these debilitating conditions.
Advances in nanotechnology are playing a crucial role in enhancing gene therapy efficacy by facilitating the targeted delivery of drugs or therapeutic agents directly to damaged brain tissue. This targeted approach ensures that the treatment reaches the affected areas with precision, maximizing its therapeutic impact on neurological disorders (Foothills Neurology).
Brain-Computer Interfaces
The evolution of brain-computer interfaces (BCIs) represents a groundbreaking development in neurology, enabling direct communication between the brain and a computer. BCIs have the potential to revolutionize the treatment of conditions such as paralysis, epilepsy, and chronic pain by providing a direct interface for neural signaling.
By harnessing the power of BCIs, individuals with neurological disorders can regain control and independence through innovative technologies that translate brain signals into actionable commands. The future of BCIs holds promise for enhancing the quality of life for patients facing motor impairments and communication challenges.
Virtual Reality Therapy Benefits
Virtual reality therapy is poised to become a mainstream treatment option in 2024 for neurological disorders such as anxiety, PTSD, and phobias. By leveraging immersive virtual environments to simulate real-life situations, virtual reality therapy desensitizes patients to triggers and helps them overcome anxiety-inducing scenarios (Foothills Neurology).
The benefits of virtual reality therapy extend beyond traditional treatment approaches, offering a safe and controlled environment for patients to confront their fears and anxieties. As technology continues to advance, virtual reality therapy is expected to play a significant role in augmenting existing therapeutic strategies for neurological conditions.
These promising advances in neurology underscore the innovative approaches and technologies that are reshaping the landscape of neurological care. By embracing gene therapy prospects, brain-computer interfaces, and virtual reality therapy benefits, the field of neurology is paving the way for transformative treatments and breakthroughs in the management of neurological disorders.
Lifestyle Modifications for Brain Health
Maintaining optimal brain health encompasses various lifestyle modifications that play a crucial role in promoting cognitive function and overall well-being. Key aspects include physical activity, quality sleep, and nutrition tailored to support brain function.
Impact of Physical Activity
Physical activity has emerged as a vital component in enhancing brain health and combating cognitive decline. Research highlighted in Frontiers in Aging Neuroscience underscores the profound effects of different modes of physical activity on cognitive function. Light to moderate exercise has been shown to slow cognitive decline and improve behavioral issues in individuals with mild cognitive impairment (MCI) and Alzheimer’s disease (AD).
Several studies have also demonstrated the positive impact of physical activity in pre-clinical models of neurodegenerative diseases such as Alzheimer’s disease (AD) and Parkinson’s disease (PD). Additionally, engaging in consistent physical activity has been linked to modifying risk factors for cardiovascular disease, obesity, and type II diabetes mellitus (T2DM) according to epidemiological research.
In the case of multiple sclerosis (MS), studies have indicated that structured exercise programs are not only safe but also effective in improving symptoms, restoring function, and enhancing the quality of life for individuals living with this condition.
Importance of Quality Sleep
Quality sleep is another critical lifestyle factor that significantly influences brain health. Adequate and restful sleep plays a fundamental role in cognitive function, memory consolidation, and overall brain performance. Disrupted sleep patterns or chronic sleep deprivation can impair cognitive abilities, affect mood regulation, and contribute to long-term neurological health issues.
Ensuring a consistent sleep schedule, creating a conducive sleep environment, and practicing relaxation techniques before bedtime can all contribute to a restorative and restful night’s sleep. Prioritizing quality sleep hygiene habits can have a positive impact on cognitive function and overall brain health.
Nutrition for Brain Function
Nutrition plays a vital role in supporting brain function and enhancing cognitive performance. Consuming a balanced diet rich in nutrients, antioxidants, and essential fatty acids can provide the brain with the necessary fuel to function optimally. Foods such as fatty fish, nuts, seeds, fruits, vegetables, and whole grains are known to promote brain health.
Incorporating brain-boosting nutrients like omega-3 fatty acids, antioxidants, vitamins, and minerals into your diet can help protect brain cells, improve memory retention, and enhance overall cognitive function. Additionally, staying hydrated and limiting the intake of processed foods, sugary snacks, and unhealthy fats can further support brain health.
By implementing lifestyle modifications such as engaging in regular physical activity, prioritizing quality sleep, and adopting a nourishing diet rich in brain-healthy nutrients, individuals can proactively support their brain health and potentially reduce the risk of neurological disorders while promoting overall well-being.
Real-world Implications & Future Trends
In the realm of neurology, understanding the real-world implications and future trends plays a crucial role in shaping the landscape of neurological disorders and treatments. Let’s delve into the World Health Organization’s perspective on neurological health, the impact of physical activity in neurodegenerative diseases, and the role of exercise in disease prevention.
World Health Organization’s Perspective
The World Health Organization (WHO) recognizes the significance of neurological disorders in global health. By highlighting the burden of neurological conditions and promoting awareness, WHO aims to mobilize resources and drive initiatives for improved neurological care worldwide. Their efforts encompass a comprehensive approach to address neurological diseases, from early detection to personalized treatment strategies.
Physical Activity in Neurodegenerative Diseases
Physical activity has emerged as a fundamental lifestyle modification with the potential to combat cognitive decline and neurodegeneration, especially in the absence of disease-modifying therapies for neurodegenerative diseases. Studies have shown that long-term adherence to exercise can be challenging for patients with chronic conditions such as Parkinson’s disease and Alzheimer’s disease (Frontiers in Aging Neuroscience).
Various forms of physical activity, including high-intensity treadmill exercise, moderate-intensity activities following WHO recommendations, and even low-impact exercises like Tai Chi, have proven beneficial in improving motor and non-motor symptoms in patients with Parkinson’s disease. The positive effects of physical activity extend beyond symptom management, contributing to overall well-being and quality of life for individuals affected by neurodegenerative diseases.
Role of Exercise in Disease Prevention
Numerous studies have underscored the preventive effects of exercise in mitigating the risk of neurodegenerative diseases. Regular physical activity has been shown to reduce the expression of amyloid-β, enhance synaptic activity, and improve mitochondrial function in pre-clinical models of Alzheimer’s and Parkinson’s diseases. These physiological changes contribute to the preservation of cognitive function, memory, and overall brain health (Frontiers in Aging Neuroscience).
Furthermore, epidemiological research has highlighted the modulatory impact of physical activity on conditions such as cardiovascular diseases, obesity, and type II diabetes mellitus. Engaging in greater levels of physical activity has been associated with a reduced risk of developing these conditions, emphasizing the potential of exercise as an adjunct therapy for disease prevention and modification.
By recognizing the importance of physical activity and incorporating it into daily routines, individuals can proactively support their brain health and reduce the risk of neurological disorders. The convergence of scientific research, global health initiatives, and individual lifestyle choices paves the way for a brighter future in combating neurological challenges through proactive measures and holistic approaches.
- About the Author
- Latest Posts
Johnnie D. Jackow Sr., the founder and CEO of Total Body Fitness, Worldwide, has a long-standing career in the fitness industry. He began as a certified personal trainer in the mid-90s and soon after authored his first weight loss book in 1998. This led to the launch of Total Body Fitness, Nationwide in the USA at the same time. Johnnie gained recognition as the fitness guru of his time, running infomercials on local TV late at night in Houston, Texas. Over the years, he has helped more than 40,000 individuals from all over the world achieve their health and fitness goals. With over 60,000 hours of documented training in integrative functional medicine, he completed his PhD in human physiology in 2010. His primary objective is to assist people in reaching their health and fitness goals through alternative approaches rather than relying solely on conventional medicine and pharmaceutical drugs. Today, with almost three decades of experience under his belt, Johnnie continues to be a leader in health and fitness.