Understanding Heart Function
Understanding heart function is essential for appreciating the complexities of cardiovascular physiology. This section covers the anatomy of the heart and the specific role of its chambers.
Anatomy of the Heart
The heart is a muscular organ that works tirelessly, pumping blood through a network of blood vessels called arteries and veins, collectively known as the cardiovascular system. The heart is composed of four chambers: two atria and two ventricles (MedicineNet).
Components of the Heart
- Atria: The two upper chambers, known as the atria, receive blood that returns to the heart.
- Ventricles: The two lower chambers, known as ventricles, pump blood out of the heart to the lungs and other parts of the body.
The heart’s structure also includes:
- Valves: Four valves that regulate blood flow through the heart’s chambers.
- Walls: The heart walls, made of three layers (epicardium, myocardium, and endocardium), contract and relax to pump blood.
- Septum: A dividing wall that separates the left and right sides of the heart.
- Coronary Arteries: Vessels that supply the heart tissue itself with oxygen and nutrients.
- Nerve Tissue: Nerve fibers that help regulate the heartbeat.
| Heart Components | Number | Function |
|---|---|---|
| Chambers | 4 (2 atria, 2 ventricles) | Receive and pump blood |
| Valves | 4 | Control blood flow direction |
| Layers of Walls | 3 (epicardium, myocardium, endocardium) | Contract and relax to pump blood |
For more details on the heart’s role within the vascular system, see vascular system adaptation.
Role of Heart Chambers
The heart chambers are pivotal in maintaining efficient blood flow dynamics.
Atria
- Right Atrium: Receives deoxygenated blood from the body via the superior and inferior vena cava.
- Left Atrium: Takes in oxygenated blood from the lungs through the pulmonary veins.
Ventricles
- Right Ventricle: Pumps deoxygenated blood to the lungs for oxygenation through the pulmonary artery.
- Left Ventricle: Pumps oxygenated blood to the rest of the body via the aorta.
The rhythmic contractions of the heart’s chambers are initiated by electrical impulses originating from specific nodes within the heart. This system ensures that blood is efficiently moved through the cardiovascular system.
These processes are tightly coordinated with other systems to maintain homeostasis, including regulating the heart rate and managing blood pressure (Cleveland Clinic). Visit blood pressure regulation for more information.
Understanding the anatomy and function of heart chambers provides a foundational knowledge needed to appreciate the overall heart function and blood flow dynamics within the human body. For further insights into how heart conditions affect this system, explore cardiac disease mechanisms.
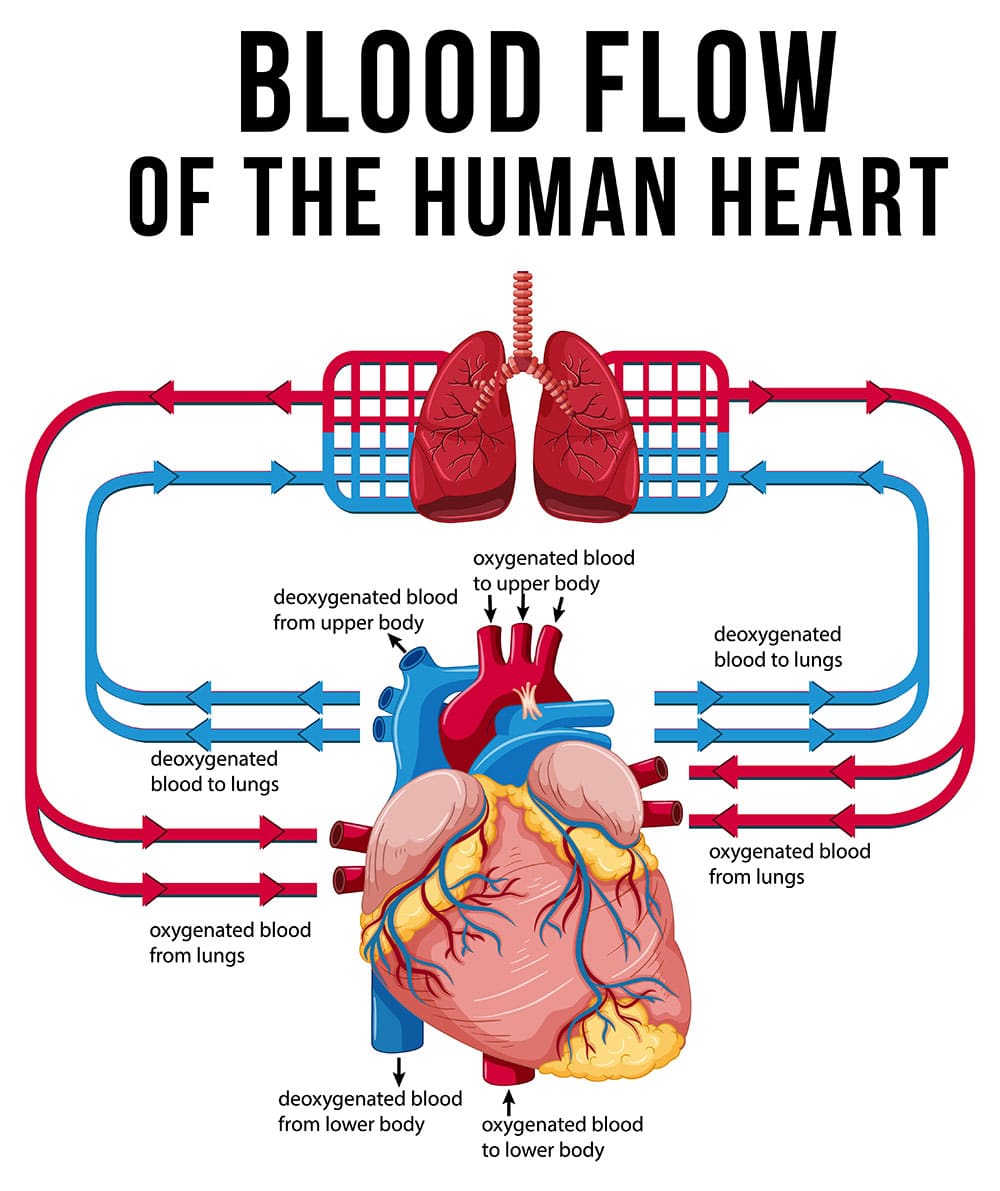
Blood Flow Dynamics
Understanding the dynamics of blood flow is essential to grasping human cardiovascular physiology. The intricate processes involved in oxygen delivery and the systemic and pulmonary circulation are key to maintaining body functionality.
Oxygen Delivery Process
The oxygen delivery process is an essential aspect of heart function and blood flow dynamics. Oxygen-rich blood is transported throughout the body, while carbon dioxide and other waste products are removed. This continuous cycle sustains cellular metabolism and overall bodily functions.
- The heart pumps oxygen-rich blood into the aorta.
- Blood travels through larger arteries, then smaller arteries, and finally into the capillary network.
- Nutrients and oxygen are delivered to tissues, while waste products are collected in veins.
- Veins return the blood to the heart for reoxygenation in the lungs.
Pulmonary and Systemic Circulation
The human blood circulatory system consists of two main circuits: systemic circulation and pulmonary circulation (NCBI Bookshelf).
Systemic Circulation
During systemic circulation, the heart propels oxygenated blood into the body’s tissues and organs.
- Left Ventricle: The heart’s left ventricle pumps oxygen-rich blood into the aorta.
- Arteries: The blood travels through a network of arteries, supplying tissues with oxygen and nutrients.
- Capillaries: Blood reaches capillaries, where oxygen and nutrients are exchanged for carbon dioxide and waste products.
- Veins: Deoxygenated blood is transported back to the heart via veins for reoxygenation.
Pulmonary Circulation
Pulmonary circulation involves the exchange of gases in the lungs (NCBI Bookshelf).
- Right Ventricle: The right ventricle pumps deoxygenated blood into the pulmonary artery.
- Pulmonary Arteries: Blood travels through pulmonary arteries and branches into smaller arteries and capillaries.
- Gas Exchange: In the capillary network around pulmonary vesicles, carbon dioxide is released and oxygen is absorbed into the bloodstream.
- Pulmonary Veins: Oxygenated blood returns to the heart, specifically the left atrium, to be pumped into systemic circulation.
| Circulation Type | Pathway | Main Function |
|---|---|---|
| Systemic Circulation | Left Ventricle → Aorta → Arteries → Capillaries → Veins → Right Atrium | Delivers oxygen and nutrients to the body |
| Pulmonary Circulation | Right Ventricle → Pulmonary Artery → Arteries → Capillaries → Pulmonary Veins → Left Atrium | Oxygenates blood and removes CO2 |
Understanding these processes provides insight into how the cardiovascular system regulates blood pressure and adapts to various physiological demands (vascular system adaptation).
Regulation of Blood Pressure
Understanding blood pressure is critical to grasping the overall heart function and blood flow dynamics. Blood pressure regulation primarily involves systolic and diastolic pressure, along with mean arterial pressure and cardiac output.
Systolic and Diastolic Pressure
Systolic and diastolic pressures are key components of arterial blood pressure. Systolic pressure, the higher value, typically around 120 mm Hg, occurs when the heart contracts and pumps blood into the arteries. Diastolic pressure, usually about 80 mm Hg, is the lower value and happens when the heart relaxes between beats (Source).
| Measurement | Normal Value (mm Hg) |
|---|---|
| Systolic | 120 |
| Diastolic | 80 |
Understanding these values is vital for diagnosing and managing conditions related to blood pressure regulation.
Mean Arterial Pressure and Cardiac Output
Mean arterial pressure (MAP) represents the average pressure in the arteries during one cardiac cycle. It can be calculated using the formula:
[ MAP = Diastolic\ Pressure + \frac{1}{3} \times (Systolic\ Pressure – Diastolic\ Pressure) ]
For example, with a systolic pressure of 120 mm Hg and a diastolic pressure of 80 mm Hg, the MAP would be:
[ MAP = 80 + \frac{1}{3} \times (120 – 80) = 80 + \frac{1}{3} \times 40 = 93.3 \ mm\ Hg ]
| Parameter | Example Value (mm Hg) |
|---|---|
| Systolic | 120 |
| Diastolic | 80 |
| MAP | 93.3 |
Cardiac output (CO), measuring how much blood the heart pumps through the ventricles per minute, is another crucial factor. It is calculated as:
[ CO = Heart\ Rate \times Stroke\ Volume ]
Factors like sympathetic stimulation, epinephrine, norepinephrine, and other hormones influence cardiac output and blood pressure, subsequently affecting blood flow.
For a deeper dive into these metrics, refer to more detailed content on vascular system adaptation and blood pressure regulation.
Understanding these concepts provides a comprehensive insight into the cardiovascular system, pivotal for health enthusiasts and professionals alike.
Hemodynamics in Cardiovascular Physiology
Understanding hemodynamics is crucial to grasp how blood moves throughout the circulatory system and supports overall heart function and blood flow dynamics. Key components of hemodynamics include vascular compliance and resistance, as well as the importance of maintaining laminar blood flow.
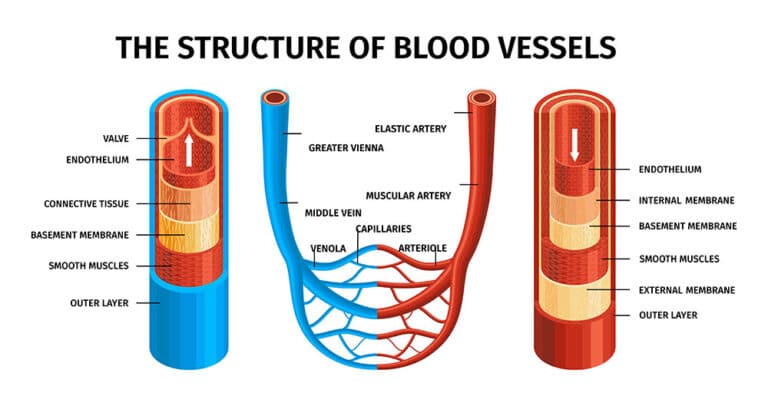
Vascular Compliance and Resistance
Vascular compliance refers to the ability of a blood vessel to expand and contract with changes in pressure. High compliance means that a vessel can accommodate varying volumes of blood with minimal changes in pressure, whereas low compliance indicates stiffness, which can increase pressure and resistance within the vessel.
Resistance in blood vessels is primarily influenced by the vessel diameter. A decrease in diameter leads to increased resistance and decreased blood flow. Factors that can affect vascular compliance include vascular diseases that cause stiffening of arteries, resulting in increased resistance, higher pressure, and more turbulent blood flow.
| Parameter | Description |
|---|---|
| Compliance | Ability of vessels to expand or contract |
| Resistance | Opposition to blood flow within a vessel |
| Diameter | Smaller diameter increases resistance |
| Disease Impact | Stiffening leads to higher resistance |
For more on how the body adapts to different vascular conditions, explore vascular system adaptation.
Importance of Laminar Blood Flow
Laminar blood flow pertains to the smooth, orderly movement of blood through the vessels, typically seen in healthy circulatory systems. It is characterized by concentric layers of blood that move parallel to each other, reducing friction and minimizing endothelial damage.
The advantages of maintaining laminar flow include reduced risk of atherosclerosis (plaque buildup in arteries) and decreased likelihood of clot formation. Laminar flow is particularly important in large arteries, where turbulent flow can lead to vascular issues and increase cardiac workload.
Turmoil within the vascular system can lead to turbulent flow, which is often observed in regions where vessels narrow or branch out at sharp angles. Ensuring healthy vessel conditions and maintaining optimal pressure play a critical role in preserving laminar blood flow and overall cardiovascular health.
Explore more on blood pressure regulation and how it affects laminar versus turbulent flow.
By understanding the elements of vascular compliance, resistance, and the necessity of laminar flow, individuals can gain deeper insight into cardiovascular physiology and the intricate dynamics of blood flow that’s vital for maintaining heart health. For additional information on the mechanisms that can lead to cardiac disease, read our article on cardiac disease mechanisms.
Capillary Function
Capillary Exchange Processes
Capillaries are the smallest blood vessels and play a crucial role in the heart function and blood flow dynamics. These microvessels facilitate the exchange of gases, nutrients, and waste products between the blood and tissue cells through processes like diffusion, filtration, and osmosis.
In diffusion, substances move from areas of higher concentration to lower concentration. This process enables oxygen and nutrients to leave the blood at one end of the capillary and waste products to be absorbed back at the other end.
The capillary network around the pulmonary vesicles is essential for gas exchange. Here, carbon dioxide is released from the blood into the air inside the vesicles, while fresh oxygen is taken up into the bloodstream (NCBI Bookshelf). This function is vital for maintaining the body’s oxygen supply and removing metabolic waste.
Blood Flow in Arteries and Capillaries
Blood flow through the cardiovascular system follows a path of decreasing pressure gradients, starting from the arteries, moving to the capillaries, and then to the veins. As blood transitions from arteries to capillaries, the flow rate decreases substantially, which is necessary for effective gas and nutrient exchange in the tissues.
| Blood Vessel Type | Pressure Gradient | Cross-Sectional Area | Blood Flow Velocity |
|---|---|---|---|
| Arteries | High | Small | Fast |
| Capillaries | Low | Large | Slow |
| Veins | Low | Moderate | Moderate |
Due to their larger cross-sectional area, the velocity of blood flow in capillaries is the slowest. This slow flow allows sufficient time for the exchange processes to occur effectively.
Understanding the dynamics of blood flow in arteries and capillaries is vital for comprehending overall cardiovascular physiology. It’s also essential to recognize how abnormalities in this flow can contribute to conditions like hypertension and heart disease. For more on how our vascular system adapts, visit our page on vascular system adaptation. To dive deeper into the regulatory mechanics, explore our article on blood pressure regulation. Additionally, for insights into disease mechanisms, check out our section on cardiac disease mechanisms.
Heart Valve Disease Overview
Heart valve disease arises when one or more of the heart valves do not function correctly, impacting blood flow dynamics and potentially leading to significant health issues.
Impact on Heart Function
When heart valves malfunction, it obstructs the normal flow of blood through the heart and to the rest of the body. The primary impact on heart function includes:
-
Increased Strain on the Heart: Conditions like valvular stenosis (narrowing of the valve) and valvular insufficiency (leaky valves) force the heart to work harder to pump blood. This can lead to symptoms such as chest pain, fatigue, dizziness, and weakness. Over time, this can reduce the heart’s efficiency and overall function (Cleveland Clinic).
-
Stenosis and Regurgitation: Stenosis causes a narrowing of the valve, restricting blood flow. Regurgitation, on the other hand, involves backward blood flow due to a valve not closing properly. Both conditions disturb the unidirectional blood flow, leading to inadequate oxygen supply to tissues and organs (Mayo Clinic).
-
Valve Prolapse: This involves the valve flaps bulging backward, potentially leading to improper sealing. While often less severe than stenosis or regurgitation, it can still cause significant complications if left untreated.
Table: Symptoms and Heart Valve Disease Impact
| Symptom | Potential Impact on Heart |
|---|---|
| Chest Pain | Increased strain and possible heart failure risk |
| Fatigue | Reduced pumping efficiency leading to less blood flow |
| Dizziness | Insufficient blood flow to the brain |
| Weakness | Poor oxygen delivery to muscles by the compromised heart |
Causes and Risk Factors
Several factors contribute to the development of heart valve disease, influencing its onset and severity:
-
Aging: With age, the heart valves may thicken and stiffen, increasing the risk of conditions like stenosis. Older individuals are more likely to develop heart valve disease due to normal wear and tear on the heart (Mayo Clinic).
-
History of Heart Conditions: Previous heart conditions, including heart attacks or other cardiovascular diseases, can damage the heart valves and increase the likelihood of disease.
-
Infections: Conditions such as rheumatic fever or endocarditis (infection of the inner heart lining) can cause significant damage to the heart valves. Prompt treatment of such infections is crucial to prevent lasting valve damage.
-
Congenital Heart Valve Disease: Some individuals are born with malformed valves, which can predispose them to early or progressive heart valve disease throughout life (Mayo Clinic).
Table: Risk Factors for Heart Valve Disease
| Risk Factor | Description |
|---|---|
| Aging | Valves thicken, harden with age |
| History of Cardiovascular Diseases | Prior heart conditions causing valve damage |
| Infections | Damaging infections like rheumatic fever or endocarditis |
| Congenital Defects | Born with valve abnormalities |
Heart valve disease significantly affects heart function and overall health. Understanding the symptoms and risk factors can help in the early diagnosis and management of this condition. For more detailed information about cardiovascular physiology, visit our article on cardiac disease mechanisms.
- About the Author
- Latest Posts
Johnnie D. Jackow Sr., the founder and CEO of Total Body Fitness, Worldwide, has a long-standing career in the fitness industry. He began as a certified personal trainer in the mid-90s and soon after authored his first weight loss book in 1998. This led to the launch of Total Body Fitness, Nationwide in the USA at the same time. Johnnie gained recognition as the fitness guru of his time, running infomercials on local TV late at night in Houston, Texas. Over the years, he has helped more than 40,000 individuals from all over the world achieve their health and fitness goals. With over 60,000 hours of documented training in integrative functional medicine, he completed his PhD in human physiology in 2010. His primary objective is to assist people in reaching their health and fitness goals through alternative approaches rather than relying solely on conventional medicine and pharmaceutical drugs. Today, with almost three decades of experience under his belt, Johnnie continues to be a leader in health and fitness.