Understanding Heart Disease
Heart disease is a complex and multifaceted condition. It is essential to understand both the risk factors and the impact of lifestyle choices to grasp the mechanisms underlying cardiac health.
Risk Factors for Heart Disease
Heart disease arises from a combination of genetic, lifestyle, and environmental factors. Key risk factors include high blood pressure, unhealthy cholesterol levels, tobacco use, and a sedentary lifestyle.
High Blood Pressure: This condition affects nearly 47% of Americans (CDC). High blood pressure can damage the heart, kidneys, brain, and other organs.
Unhealthy Blood Cholesterol Levels: Elevated cholesterol can lead to a buildup in artery walls, narrowing the arteries and reducing blood flow to crucial organs like the heart, brain, and kidneys (CDC).
Tobacco Use: Smoking increases the risk of heart disease by damaging the heart and blood vessels, raising blood pressure, and reducing the oxygen-carrying capacity of blood (CDC).
Genetic Factors: Some populations, such as those of South Asian, African, or Caribbean descent, have a statistically higher risk of cardiovascular disease. Genetic factors contribute to unexplained cases of heart failure, known as idiopathic cardiomyopathy.
| Risk Factor | Prevalence |
|---|---|
| High Blood Pressure | 47% |
| Elevated Cholesterol | Varies |
| Tobacco Use | Significant |
| Genetic Predisposition | Higher in specific populations |
| Sedentary Lifestyle | Common |
Impact of Lifestyle Factors
The choices individuals make daily have a substantial impact on heart health. Adopting healthy habits can mitigate many risk factors for heart disease.
Physical Activity: Regular exercise is crucial for maintaining heart function and blood flow dynamics. Physical activity helps in managing weight, reducing blood pressure, and improving cholesterol levels.
Diet: A balanced diet low in saturated fats, trans fats, and cholesterol helps maintain healthy cholesterol levels. Including fruits, vegetables, whole grains, and lean proteins supports cardiovascular wellness.
Smoking Cessation: Avoiding tobacco and quitting smoking can significantly reduce the risk of heart disease. Tobacco use damages the cardiovascular system and raises blood pressure.
Managing Stress: Chronic stress can contribute to heart disease. Effective stress management techniques, such as mindfulness and exercise, can promote better heart health.
Alcohol Consumption: Limiting alcohol intake can also help maintain healthy blood pressure and reduce the risk of cardiovascular complications.
| Lifestyle Factor | Benefit |
|---|---|
| Regular Physical Activity | Improves blood flow, reduces blood pressure |
| Balanced Diet | Maintains cholesterol, supports overall health |
| Smoking Cessation | Reduces risk of cardiovascular disease |
| Stress Management Techniques | Promotes better heart health |
| Limited Alcohol Intake | Maintains healthy blood pressure |
By understanding the intricate relationship between risk factors and lifestyle choices, health enthusiasts can adopt and advocate for habits that support cardiovascular health. For more detailed insights, explore topics like blood pressure regulation.
Atherosclerosis and Cardiovascular Health
The Development of Atherosclerosis
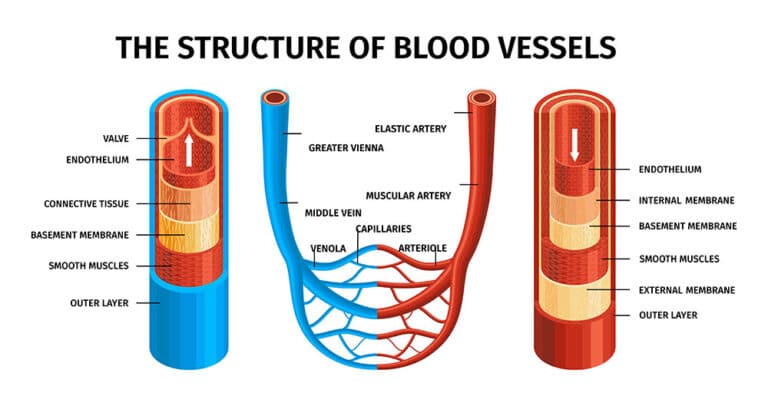
Atherosclerosis is the build-up of plaques in the arterial walls, a process that can take many years to manifest. According to the U.S. National Institutes of Health, about half of people aged 45 to 84 in America have atherosclerosis without being aware of it. This condition begins with damage to the endothelium, the inner lining of the artery Cleveland Clinic.
Several risk factors contribute to endothelial injury:
- High blood pressure
- High cholesterol
- Smoking
- Diabetes
When the endothelium is damaged, cholesterol, fats, and other substances accumulate to form plaques. As plaques grow, they can restrict blood flow or even rupture, leading to blood clots.
| Age Group | Percentage with Atherosclerosis |
|---|---|
| 45-54 | 40% |
| 55-64 | 55% |
| 65-74 | 65% |
| 75-84 | 75% |
Consequences of Atherosclerosis
Atherosclerosis can lead to severe health complications, making it the leading cause of death worldwide. Some consequences include:
- Heart Attacks: Blocked arteries can stop oxygen-rich blood from reaching the heart.
- Strokes: Plaques or clots in the arteries leading to the brain can cause strokes.
- Peripheral Artery Disease: Reduced blood flow to limbs can result in pain and mobility issues.
Atherosclerosis symptoms may develop gradually as plaques build up, with variations depending on the affected artery. Severe signs and symptoms may occur when a major artery is blocked, such as those seen in heart attacks, strokes, or blood clots.
Management and Treatment Options
Treating atherosclerosis involves a combination of lifestyle changes, medications, and surgical interventions to reduce risk factors and prevent complications.
Lifestyle Changes
Adopting healthier habits can significantly lower the risk of developing atherosclerosis:
- Dietary Recommendations: A diet low in saturated fats, cholesterol, and sodium.
- Physical Activity: Regular exercise to maintain cardiovascular health. Visit our article on the importance of physical activity for more details.
- Smoking Cessation: Eliminating tobacco use to reduce arterial damage.
Medications
Medications can help manage risk factors and slow the progression of atherosclerosis:
- Statins: Lower cholesterol levels.
- Antihypertensives: Control high blood pressure.
- Antiplatelets: Prevent blood clots.
Surgical Procedures
In severe cases, surgical intervention may be necessary:
- Coronary Angioplasty: Opens narrowed arteries.
- Coronary Artery Bypass: Creates an alternative route for blood flow.
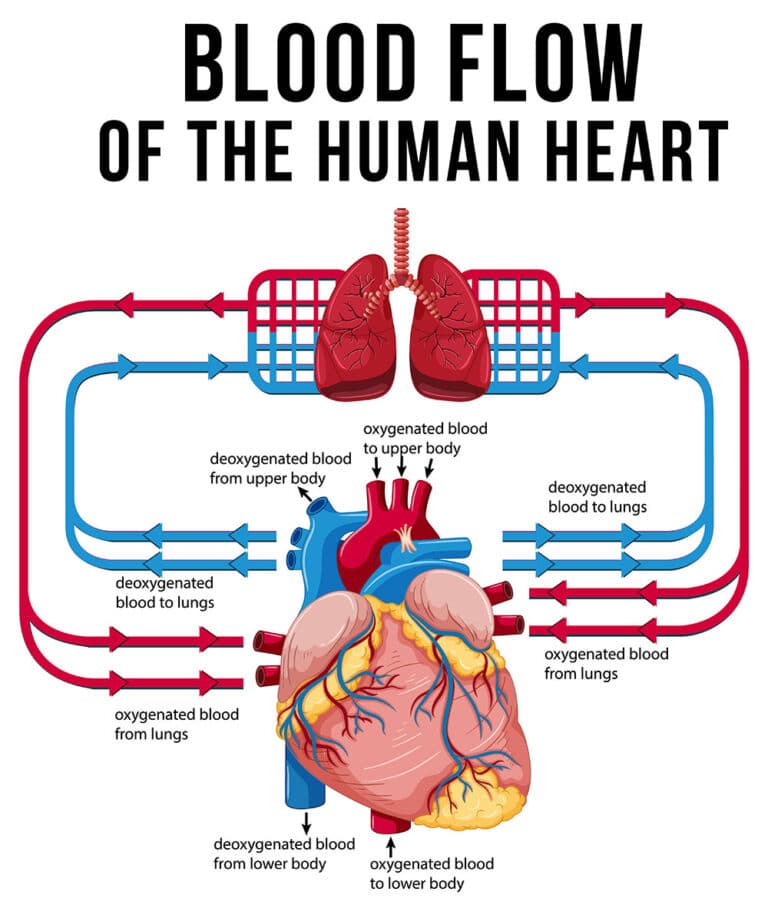
By understanding the heart function and blood flow dynamics, individuals can better appreciate the importance of managing atherosclerosis. For further insights into vascular system adaptation and blood pressure regulation, check out our related articles.
Genetic Influence on Cardiovascular Health
Understanding the genetic influence on cardiovascular health is pivotal in comprehending the broader spectrum of cardiac disease mechanisms. Genetics play a significant role, not just in the risk of developing heart conditions, but also in the management and treatment approaches.
Role of Genetics in Heart Disease
Genetics play a key role in the development of cardiovascular diseases. Family history is a recognized risk factor. If a person’s first-degree relative developed cardiovascular disease at a relatively young age, it increases the individual’s risk. For example:
- If a person’s father or brother developed CVD before age 55.
- If a person’s mother or sister developed CVD before age 65.
Idiopathic cardiomyopathy, a condition where the heart muscles become abnormal without any identified cause, can also have genetic underpinnings. About one-quarter of such cases are thought to have specific genetic causes (Henry Ford Health).
| Risk Factors | Impact on Cardiovascular Disease |
|---|---|
| Family History (early CVD) | Increases risk significantly |
| Idiopathic Cardiomyopathy | ~25% linked to genetics |
| Coronary Artery Disease (CAD) | 50% risk set at birth by genetic makeup |
Genetic Testing for Cardiovascular Conditions
Genetic testing provides insights into the inherited components of heart disease. While consumer genetic testing services like 23andMe® and Ancestry.com® are popular, they should be approached with caution. These tests are not designed to diagnose genetic conditions and should not be solely relied upon for health decisions.
For accurate genetic assessments, specialized tests performed under medical supervision are recommended. These tests can help identify specific genetic mutations associated with cardiovascular conditions, thereby informing a more tailored approach to prevention and treatment.
In coronary artery disease (CAD), studies indicate that 50% of the risk is determined by genetic makeup, with the remaining 50% influenced by lifestyle factors (Nebraska Medicine). Understanding one’s genetic predisposition can lead to better management strategies, integrating both genetic and lifestyle modifications. For more on how lifestyle affects cardiovascular health, see our section on Lifestyle Modifications for Heart Health.
Integrating genetic testing with regular health assessments might help in early detection and personalized management of cardiovascular diseases. To understand the details of heart function and blood flow dynamics and blood pressure regulation, readers may explore linked resources.
Diabetes and Cardiovascular Complications
Heart disease and diabetes are closely linked, with diabetes playing a significant role in the development of cardiovascular complications. Understanding how these conditions intersect is crucial for managing and preventing heart disease in individuals with diabetes.
Connection Between Diabetes and Heart Disease
Diabetes is strongly associated with both macrovascular and microvascular disease, impacting large arteries and small arteries and capillaries (NCBI). Chronic hyperglycemia, or high blood sugar, and insulin resistance are significant factors in the initiation of these vascular complications. Adults with diabetes are nearly twice as likely to have heart disease or stroke compared to adults without diabetes (NIDDK).
| Condition | Relative Risk of Heart Disease |
|---|---|
| Diabetes | 2x |
| No Diabetes | 1x |
Furthermore, diabetes-related vascular disease increases the risk of cardiovascular events and all-cause mortality. For more insight into how blood flow dynamics are affected, visit heart function and blood flow dynamics.
Mechanisms Leading to Vascular Complications
Several mechanisms contribute to the vascular complications observed in individuals with diabetes:
- Advanced Glycation End Products (AGEs):
- Patients with diabetes exhibit increased tissue and circulating concentrations of AGEs and soluble RAGE, which are predictive of cardiovascular events (NCBI). These biomarkers can be used to monitor the progression of vascular disease in diabetic patients.
- Oxidative Stress:
- Chronic hyperglycemia leads to elevated oxidative stress, damaging blood vessels and promoting inflammation.
- Inflammation:
- Persistent inflammation is a crucial factor in the development of diabetes-related cardiovascular issues. New therapeutic approaches target oxidative stress and inflammation to mitigate these effects.
| Mechanism | Impact on Vascular Health |
|---|---|
| AGEs | Increase cardiovascular risk |
| Oxidative Stress | Damages blood vessels |
| Inflammation | Promotes vascular issues |
- Insulin Resistance:
- Insulin resistance, often detectable years before the onset of Type 2 Diabetes, is associated with obesity and hypertension. Such factors exacerbate cardiovascular risks (NCBI).
Therapeutic development is ongoing, with drugs like linagliptin and Nox inhibitors showing potential in reducing these vascular complications. Individuals with diabetes should consult healthcare providers for strategies to manage blood sugar levels and reduce cardiovascular risks.
For further information on how the vascular system adapts to these conditions, visit vascular system adaptation. Understanding these connections underscores the importance of targeted interventions and lifestyle modifications to mitigate the impact of diabetes on cardiovascular health.
Lifestyle Modifications for Heart Health
Lifestyle changes play a pivotal role in mitigating the risk factors associated with cardiovascular diseases. Below are essential modifications for enhancing cardiovascular wellness.
Importance of Physical Activity
Physical inactivity remains a notable risk factor for cardiovascular disease. Regular exercise helps reduce the risk of obesity, high blood pressure, and other conditions contributing to heart diseases. Experts recommend engaging in 150 minutes of moderate to high-intensity exercise per week for significant health benefits. This can be achieved through activities such as brisk walking, cycling, or swimming.
| Activity | Duration Per Week |
|---|---|
| Brisk Walking | 150 minutes |
| Cycling | 150 minutes |
| Swimming | 150 minutes |
Adopting an active lifestyle can lead to improved heart function and blood flow dynamics.
Dietary Recommendations for Cardiovascular Wellness
A balanced diet rich in fruits, vegetables, and low-fat dairy products can significantly impact cardiovascular health. Lowering fat intake, limiting soda and sodium chloride consumption, and ensuring proper intake of essential vitamins and minerals are crucial for preventing cardiovascular diseases.
| Food Group | Recommendation |
|---|---|
| Fruits and Vegetables | High intake |
| Low-Fat Dairy Products | Moderate intake |
| Fatty Foods | Low intake |
| Sodium Chloride | Limited intake |
Bioactive compounds in plant foods, such as polyphenolic compounds, peptides, oligosaccharides, vitamins, and fatty acids, have cardioprotective properties (PMC). For more detailed dietary recommendations, explore our section on blood pressure regulation.
Smoking Cessation and Heart Disease Prevention
Smoking is a significant risk factor for heart disease. It is particularly crucial for individuals with diabetes to quit smoking as both conditions narrow blood vessels, increasing the risk of long-term cardiovascular complications.
| Condition | Risk |
|---|---|
| Smoking | Increased risk of heart disease |
| Diabetes | Increased risk of vascular complications |
By cessation of smoking, individuals can greatly enhance their heart health and reduce the likelihood of developing severe cardiovascular problems. Learn more about vascular system adaptation and how it impacts overall cardiovascular wellness.
Through these lifestyle modifications, individuals can take proactive steps towards preserving their heart health and preventing the development of cardiac disease mechanisms.
Cardiovascular Disease Prevention Strategies
To mitigate the risk of cardiovascular disease (CVD), several prevention strategies can be adopted. This section explores the role of omega-3 fatty acids, phenolic compounds, and genetic and familial risk factors in the context of CVD prevention.
Omega-3 Fatty Acids and Cardiovascular Health
Omega-3 fatty acids are essential fats that play a critical role in heart health. They are known for their ability to reduce inflammation, lower triglyceride levels, and improve overall cardiovascular function. Common sources of omega-3 fatty acids include fatty fish, flaxseeds, and walnuts.
Benefits of Omega-3 Fatty Acids:
- Reduced risk of arrhythmias (abnormal heartbeats)
- Decreased triglyceride levels
- Lower blood pressure
- Prevention of plaque buildup in arteries
Incorporating foods rich in omega-3 fatty acids into the diet or considering supplements can be beneficial. For more information on blood pressure regulation, visit our blood pressure regulation article.
| Omega-3 Source | Recommended Intake (g/serving) |
|---|---|
| Salmon (cook) | 1.57 |
| Flaxseeds (ground) | 2.35 |
| Walnuts | 2.57 |
Phenolic Compounds in Heart Disease Prevention
Phenolic compounds are antioxidants found in a variety of plant-based foods. They are known for their ability to neutralize free radicals, thus protecting the cardiovascular system from oxidative stress. These compounds also enhance endothelial function and reduce inflammation, key factors in preventing heart disease.
Rich Sources of Phenolic Compounds:
- Berries (blueberries, strawberries)
- Dark chocolate
- Green tea
- Red wine (in moderation)
Regular consumption of phenolic-rich foods can contribute to cardiovascular wellness. For a deeper understanding of heart function, check out our article on heart function and blood flow dynamics.
| Food Source | Phenolic Content (mg/100g) |
|---|---|
| Blueberries | 529 |
| Dark Chocolate | 450 |
| Green Tea | 330 |
Addressing Genetic and Familial Risk Factors
Genetics play a significant role in determining an individual’s risk of developing cardiovascular disease. Family history is a recognized risk factor, and certain populations have a higher predisposition to heart conditions.
Genetic Impact on Heart Health:
- If a first-degree relative (parent or sibling) developed CVD at a young age (before age 55 for males, before age 65 for females), the individual’s risk increases.
- People of South Asian, African, or Caribbean descent are statistically at higher risk for CVD (ADA).
- Rare genetic mutations can contribute to idiopathic cardiomyopathy.
Despite genetic predispositions, lifestyle choices are paramount. Individuals with good genes making poor lifestyle choices have the same coronary event risk as those with bad genes making good lifestyle choices (Nebraska Medicine). Adopting a healthy lifestyle, including regular exercise, a balanced diet, and smoking cessation, is crucial in preventing heart disease. Learn more about specific lifestyle adaptations in our article on vascular system adaptation.
For those concerned about genetic risks, genetic testing can provide insights into individual susceptibility to heart disease, allowing for proactive and personalized preventive measures.
- About the Author
- Latest Posts
Johnnie D. Jackow Sr., the founder and CEO of Total Body Fitness, Worldwide, has a long-standing career in the fitness industry. He began as a certified personal trainer in the mid-90s and soon after authored his first weight loss book in 1998. This led to the launch of Total Body Fitness, Nationwide in the USA at the same time. Johnnie gained recognition as the fitness guru of his time, running infomercials on local TV late at night in Houston, Texas. Over the years, he has helped more than 40,000 individuals from all over the world achieve their health and fitness goals. With over 60,000 hours of documented training in integrative functional medicine, he completed his PhD in human physiology in 2010. His primary objective is to assist people in reaching their health and fitness goals through alternative approaches rather than relying solely on conventional medicine and pharmaceutical drugs. Today, with almost three decades of experience under his belt, Johnnie continues to be a leader in health and fitness.