Understanding Endocrine Disorders
Endocrine disorders arise from the body’s complex hormone-producing system, which influences many vital functions. This section delves into the basics of endocrinology and examines these disorders in the human body.
Overview of Endocrinology
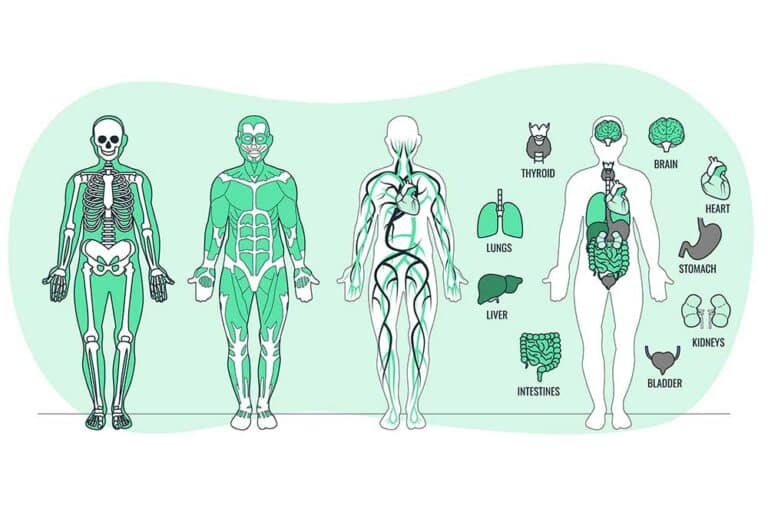
Endocrinology is the branch of medicine focused on the endocrine system, which includes glands that produce hormones. Hormones are chemical messengers that travel through the bloodstream to tissues and organs, regulating essential functions such as growth, metabolism, and reproduction. Understanding the human body endocrine system is crucial for comprehending endocrine disorders and treatments.
The endocrine system comprises several key glands:
- Pituitary Gland: Often considered the “master gland” as it controls other endocrine glands.
- Thyroid Gland: Regulates metabolism, energy production, and neurological development.
- Adrenal Glands: Produce hormones involved in stress responses and metabolic processes.
- Pancreas: Plays a vital role in glucose regulation.
For more details on the anatomy and function of these glands, see endocrine glands and their functions.
Endocrine Disorders in the Human Body
Endocrine disorders typically stem from hormone imbalances, where a gland produces either excessive or insufficient amounts of a hormone. This disruption can lead to various conditions that affect multiple aspects of health (Tampa General Hospital). Here are some common disorders:
- Diabetes: Results from issues with insulin production or action, impacting blood sugar regulation.
- Adrenal Insufficiency: Characterized by inadequate production of hormones like cortisol.
- Hyperthyroidism: An overactive thyroid gland leads to increased metabolism.
- Hypopituitarism: The pituitary gland fails to produce one or more of its hormones.
For an overview of these disorders, visit endocrine system diseases and disorders.
| Disorder | Affected Gland | Common Symptoms |
|---|---|---|
| Diabetes | Pancreas | Increased thirst, frequent urination |
| Adrenal Insufficiency | Adrenal Glands | Fatigue, muscle weakness |
| Hyperthyroidism | Thyroid Gland | Weight loss, rapid heartbeat |
| Hypopituitarism | Pituitary Gland | Fatigue, weight gain |
Impaired feedback mechanisms within the endocrine system contribute to these imbalances, impacting hormone production and action (Tampa General Hospital). Environmental factors, such as iodine deficiency leading to goitre, also play a role (Top Doctors).
Autoimmune conditions like Hashimoto thyroiditis, where the immune system attacks endocrine glands, are another common cause (Top Doctors). Exploring these conditions further can help in understanding their impact on metabolism and overall health. For more on this topic, see endocrinology and metabolism functions.
Common Endocrine Disorders
Endocrine disorders can significantly affect an individual’s health and well-being. Here, we explore some of the most common endocrine disorders and their impacts.
Diabetes and Its Impact
Diabetes is the most common endocrine disorder diagnosed in the U.S. (WebMD). It occurs when the body either does not produce enough insulin or cannot use it effectively. Insulin is a hormone produced by the pancreas that regulates blood sugar levels.
| Type | Description | Key Impacts |
|---|---|---|
| Type 1 Diabetes | Autoimmune disorder where the pancreas produces little or no insulin | Needs insulin therapy; risk of ketoacidosis |
| Type 2 Diabetes | Body becomes resistant to insulin or the pancreas does not produce enough insulin | Can lead to heart disease, nerve damage, eye problems |
| Gestational Diabetes | Occurs during pregnancy | May increase risk of type 2 diabetes later in life |
Adrenal Insufficiency
Adrenal insufficiency, including Addison’s disease, occurs when the adrenal glands do not produce enough cortisol and aldosterone. Symptoms include fatigue, stomach upset, dehydration, and skin changes. Cortisol helps the body respond to stress, while aldosterone regulates sodium and potassium levels.
| Symptom | Description |
|---|---|
| Fatigue | Extreme tiredness not relieved by rest |
| Stomach Upset | Nausea, vomiting, abdominal pain |
| Dehydration | Loss of body fluids and minerals |
| Skin Changes | Darkening of the skin, especially in scars and creases |
Hyperthyroidism Overview
Hyperthyroidism occurs when the thyroid gland produces too much thyroid hormone, leading to symptoms such as weight loss, a fast heart rate, sweating, and nervousness. Grave’s disease is the most common cause of an overactive thyroid.
| Symptom | Description |
|---|---|
| Weight Loss | Unexplained loss of weight despite normal eating habits |
| Fast Heart Rate | Increased heartbeats, which can lead to palpitations |
| Sweating | Excessive perspiration, even without physical exertion |
| Nervousness | Anxiety and irritability |
Hypopituitarism
Hypopituitarism is a condition where the pituitary gland releases little or no hormones. This can lead to various symptoms such as fatigue, loss of interest in sex, decreased appetite, and in women, cessation of menstrual periods (WebMD).
| Symptom | Description |
|---|---|
| Fatigue | Persistent tiredness and weakness |
| Low Libido | Reduced sexual drive and interest |
| Appetite Loss | Decreased desire to eat |
| Amenorrhea | Absence of menstrual periods in women |
Understanding endocrine system diseases and disorders helps in recognizing these conditions early and seeking appropriate treatment. For more insights on the endocrine system, explore our pages on human body endocrine system and the role of hormones in metabolism.
Symptoms & Diagnosis
Understanding the symptoms and diagnostic approaches for endocrine disorders is crucial. This section will provide a detailed look at how these disorders manifest and how they are diagnosed.
Recognizing Endocrine Disorder Symptoms
Symptoms of endocrine disorders can vary widely depending on the specific gland affected. However, some common symptoms are experienced across various conditions.
| Symptom | Description |
|---|---|
| Fatigue | General tiredness and lack of energy. |
| Weakness | Reduced muscle strength. |
| Weight Changes | Unexplained weight loss or gain. |
| Heart Rate Irregularities | Unusual fast or slow heartbeat. |
| Sweating | Excessive perspiration. |
| Nervousness | Anxiety or jitteriness. |
| Constipation | Difficulty in bowel movements. |
| Depression | Persistent sadness or lack of interest. |
| Infertility | Difficulty in conceiving. |
Sources: WebMD
For those experiencing symptoms like weight changes, heart rate irregularities, or constipation, consulting a healthcare provider is recommended. Certain conditions, such as autoimmune thyroiditis (Hashimoto’s), often run in families and may also present with fatigue, weakness, and depression.
Diagnostic Approaches
Diagnosing endocrine disorders involves a multifaceted approach, often starting with a comprehensive medical history and physical examination.
- Blood Tests: Fundamental for diagnosing endocrine disorders, blood tests measure hormone levels and can detect imbalances.
- TSH Levels: Critical for diagnosing thyroid disorders.
- Blood Sugar Levels: Used to diagnose diabetes.
-
Imaging Tests: These may include ultrasound, CT scans, or MRI to visualize gland structure and identify abnormalities such as tumors or nodules.
-
Urine Tests: Sometimes used to measure hormone levels over a 24-hour period.
-
Stimulation or Suppression Tests: These tests evaluate gland function by measuring how well they respond to certain stimuli or suppressive agents.
| Diagnostic Test | Purpose |
|---|---|
| Blood Tests | Measures hormone levels (e.g., TSH, blood sugar). |
| Imaging Tests | Visualizes gland structure (e.g., ultrasound, MRI). |
| Urine Tests | Measures hormone levels over time. |
| Stimulation/Suppression Tests | Evaluates gland function under specific conditions. |
Source: Upstate Medicine
To learn more about specific conditions and their diagnostic methods, explore our articles on endocrine system diseases and disorders and endocrinology and metabolism basics. For information on the human body’s endocrine system anatomy and physiology and role of hormones in metabolism, please refer to the provided links.
Causes of Endocrine Disorders
Understanding the causes of endocrine disorders is essential for diagnosing and treating these conditions. Two primary causes include hormonal imbalances and the presence of nodules and tumors.
Hormonal Imbalances
Hormonal imbalances are a leading cause of endocrine disorders. Hormones are chemical messengers produced by the endocrine glands and play a critical role in regulating various functions in the body. An imbalance, either increased or decreased levels, can lead to several health issues.
Hormonal imbalances can result from various factors such as:
- Genetics
- Infection
- Noncancerous tumors
- Inability of the endocrine feedback system to maintain proper hormone levels
Common endocrine disorders caused by hormonal imbalances include:
- Adrenal Insufficiency
- Cushing’s Disease
- Gigantism
- Hyperthyroidism
- Hypothyroidism
- Hypopituitarism
- Multiple Endocrine Neoplasia Types 1 and 2 (MEN1 and MEN2)
- Polycystic Ovary Syndrome (PCOS)
- Precocious Puberty
For more details on the role of hormones and the endocrine system’s function, visit our articles on endocrine system anatomy and physiology and role of hormones in metabolism.
| Disorder | Hormonal Imbalance |
|---|---|
| Adrenal Insufficiency | Low cortisol |
| Cushing’s Disease | High cortisol |
| Hyperthyroidism | High thyroxine |
| Hypothyroidism | Low thyroxine |
| PCOS | High androgens |
Nodules and Tumors
Nodules and tumors in the endocrine glands can disrupt normal hormone production, leading to endocrine disorders. Tumors in endocrine glands, whether benign or malignant, can alter the gland’s functionality. This can result in excessive or insufficient hormone production.
Factors contributing to the development of nodules and tumors include:
- Genetic mutations
- Hereditary components
- Environmental influences
Common tumors associated with endocrine disorders are:
- Parathyroid Tumors
- Medullary Thyroid Cancer
- Adrenal Tumors (e.g., Pheochromocytoma)
Up to 40% of cases of conditions like medullary thyroid cancer and certain adrenal tumors have a hereditary component (Top Doctors). Genetic mutations can pass from generation to generation, increasing the risk of developing these tumors.
For more information on how these factors impact hormone production and endocrine function, refer to endocrinology and metabolism basics and endocrine glands and their functions.
By understanding the causes of endocrine disorders, one can better appreciate the complexity of the endocrine system and its impact on homeostasis. Awareness and early detection are key in managing these conditions effectively.
Treatment Options
Addressing endocrine disorders and treatments involves a variety of strategies tailored to the specific condition and its impact on the body’s hormonal balance. Treatment often includes medication, lifestyle modifications, and, in some cases, surgical interventions.
Medication and Lifestyle Modifications
Medications play a crucial role in managing endocrine disorders. For example, individuals with hypothyroidism often require thyroid replacement medication to maintain normal hormone levels (Mercy). Various medications are used to treat different endocrine conditions, each targeting specific hormonal imbalances.
| Condition | Common Medication | Target |
|---|---|---|
| Hypothyroidism | Levothyroxine | Thyroid Hormone Replacement |
| Hyperthyroidism | Methimazole, Propylthiouracil | Reduce Thyroid Hormone Production |
| Diabetes Type 1 | Insulin | Regulate Blood Sugar |
| Diabetes Type 2 | Metformin, Glipizide | Increase Insulin Sensitivity |
In addition to medication, lifestyle modifications are essential. Patients are often advised to follow specific dietary plans, engage in regular physical activity, and avoid substances that could exacerbate their condition. For instance, individuals with diabetes benefit from a diet low in simple sugars and high in fiber.
Surgical Interventions
Surgical options are considered when medication and lifestyle changes are insufficient to manage the endocrine disorder. Surgery may be necessary to remove tumors, nodules, or parts of overactive glands. For example, a patient with a thyroid nodule that is causing hormone imbalances might undergo a thyroidectomy.
| Disorder | Surgical Procedure | Description |
|---|---|---|
| Hyperthyroidism | Thyroidectomy | Removal of part or all of the thyroid gland |
| Adrenal Insufficiency | Adrenalectomy | Removal of one or both adrenal glands |
| Hyperparathyroidism | Parathyroidectomy | Removal of one or more parathyroid glands |
| Pituitary Tumors | Transsphenoidal Surgery | Removal of pituitary tumor through the nasal passage |
Each surgical intervention is tailored to address the specific disruption within the endocrine system, ensuring specialized care (Tampa General Hospital). Post-surgical care often includes hormone replacement therapy and regular monitoring to maintain hormonal balance.
Effective treatment of endocrine disorders requires a combination of medication, lifestyle changes, and sometimes surgical intervention. Ongoing monitoring, patient education, and support are key to managing these conditions over the long term. For more information on how hormones regulate the body’s metabolism, visit our article on the role of hormones in metabolism.
For additional details on how the endocrine system functions, check out endocrine glands and their functions.
Preventing Endocrine Disorders
Preventive measures play a crucial role in minimizing the risk of endocrine disorders. These measures focus on early detection through routine check-ups and adopting healthy lifestyle changes.
Importance of Routine Check-Ups
Regular health evaluations are essential for the early detection and management of endocrine disorders. Adolescents, in particular, undergo significant physiological, psychological, and social changes, making routine check-ups vital. Pediatricians recommend annual visits between the ages of 11 and 21 for health evaluations and anticipatory guidance (PMC).
Routine check-ups can help identify symptoms or risk factors of endocrine disorders early, allowing for timely intervention and treatment. Such evaluations are critical in preventing complications associated with conditions like diabetes and its impact and hormonal imbalances.
| Age Group | Recommended Frequency |
|---|---|
| Adolescents (11-21) | Annual Check-Up |
| Adults (21-40) | Biennial Check-Up |
| Adults (40+) | Annual Check-Up |
Source: PMC
Impact of Lifestyle Changes
Adopting a healthier lifestyle can significantly reduce the risk of developing endocrine disorders. Key lifestyle changes include:
-
Balanced Diet: Consuming a varied diet rich in fruits, vegetables, whole grains, lean proteins, and healthy fats can help maintain hormonal balance. Avoiding excessive sugar and processed foods is crucial in preventing conditions like insulin resistance.
-
Regular Exercise: Physical activity is beneficial for overall health and aids in maintaining a healthy weight, which is essential for preventing endocrine disorders like hypopituitarism.
-
Stress Management: Chronic stress can impact hormonal balance. Techniques such as mindfulness, yoga, and deep-breathing exercises can help manage stress levels.
-
Avoiding Harmful Substances: Limiting the intake of alcohol, quitting smoking, and avoiding recreational drugs can prevent endocrine disruptions.
| Lifestyle Change | Benefits |
|---|---|
| Balanced Diet | Maintains hormonal balance |
| Regular Exercise | Reduces risk of obesity-related disorders |
| Stress Management | Prevents hormonal imbalance |
| Avoid Harmful Substances | Supports overall hormonal health |
It’s clear that proactive measures such as routine medical evaluations and mindful lifestyle adjustments can help in the prevention of endocrine disorders. Regular check-ups aid in early detection, while healthy living practices support the body’s endocrine system functions. For more insights into the endocrine system, visit our articles on endocrine system anatomy and physiology and endocrinology and metabolism basics.
- About the Author
- Latest Posts
Johnnie D. Jackow Sr., the founder and CEO of Total Body Fitness, Worldwide, has a long-standing career in the fitness industry. He began as a certified personal trainer in the mid-90s and soon after authored his first weight loss book in 1998. This led to the launch of Total Body Fitness, Nationwide in the USA at the same time. Johnnie gained recognition as the fitness guru of his time, running infomercials on local TV late at night in Houston, Texas. Over the years, he has helped more than 40,000 individuals from all over the world achieve their health and fitness goals. With over 60,000 hours of documented training in integrative functional medicine, he completed his PhD in human physiology in 2010. His primary objective is to assist people in reaching their health and fitness goals through alternative approaches rather than relying solely on conventional medicine and pharmaceutical drugs. Today, with almost three decades of experience under his belt, Johnnie continues to be a leader in health and fitness.