Kidney’s Role in Blood Pressure Regulation
The kidneys play a crucial role in maintaining the body’s blood pressure levels. They achieve this through various mechanisms, including the regulation of extracellular fluid volume and renal perfusion pressure.
Regulation of Arterial Blood Pressure
The regulation of arterial blood pressure involves the control of extracellular fluid volume, which is regulated by the kidneys. The kidneys influence blood pressure by adjusting the volume of blood plasma, which in turn affects arterial circulation.
A key component in this process is the renin-angiotensin-aldosterone system (RAAS). The RAAS regulates blood pressure by enhancing sodium reabsorption, increasing water retention, and adjusting vascular tone (Cleveland Clinic).
Here’s a simplified table for better understanding:
| Function | Mechanism |
|---|---|
| Sodium Reabsorption | Increases blood volume and pressure |
| Water Retention | Maintains blood volume |
| Vascular Tone | Adjusts blood vessel diameter |
For a detailed analysis of this system, visit our article on vascular system adaptation.
Renal Perfusion Pressure
Renal perfusion pressure is another significant factor in blood pressure regulation. Renal artery perfusion pressure directly affects the kidney’s ability to excrete sodium, a process known as pressure natriuresis. When blood pressure increases, the kidneys excrete more sodium and water, thereby lowering the blood pressure back to normal levels. Conversely, low perfusion pressure triggers sodium and water retention, raising blood pressure.
Excessive salt intake can overwhelm this system, making it difficult for the kidneys to regulate blood pressure effectively. For salt-sensitive individuals, this can lead to hypertension.
The interplay between various vasoactive systems and the kidneys highlights the complexity of blood pressure regulation:
| System | Effect on Blood Pressure |
|---|---|
| Renin-Angiotensin-Aldosterone (RAAS) | Increases BP by promoting sodium/water retention |
| Sympathetic Nervous System | Modulates vascular tone and cardiac output |
| Natriuretic Peptides | Decreases BP by promoting sodium/water excretion |
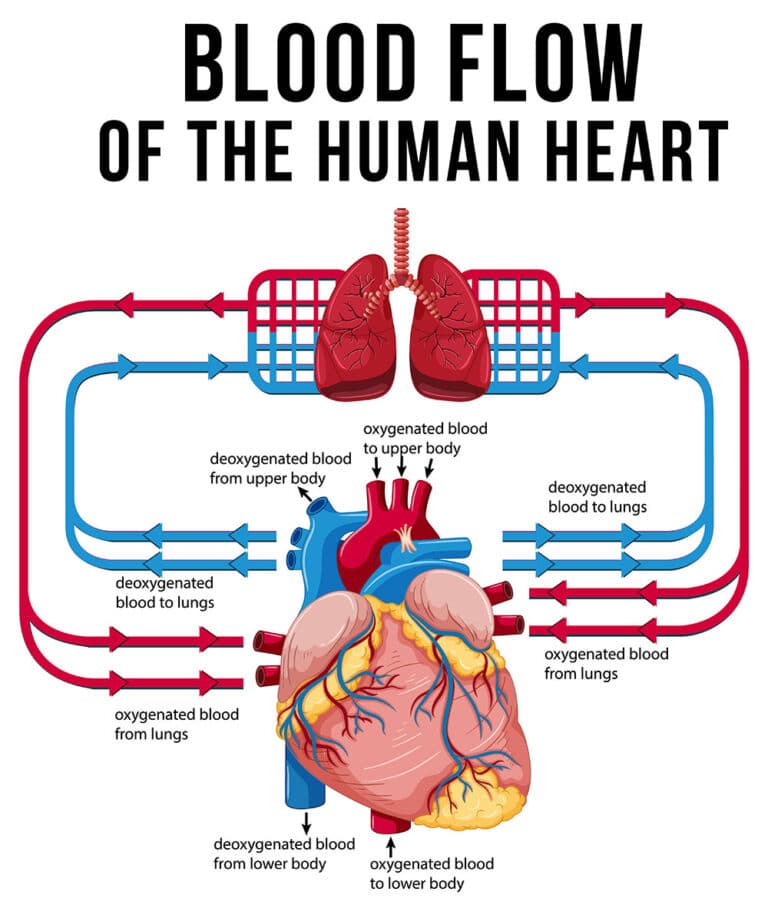
For more detailed insights on how the kidneys and cardiovascular system interact, refer to our article on heart function and blood flow dynamics.
Understanding these mechanisms provides a comprehensive view of how the kidneys maintain blood pressure, offering valuable insights into conditions like hypertension and hypotension. For further reading, you can explore various aspects of cardiac disease mechanisms that impact kidney function and blood pressure.
Impact of Hypertension on Kidney
Hypertension, commonly known as high blood pressure, has a significant impact on kidney function. Understanding the intricate relationship between the kidneys and blood pressure highlights the importance of kidney health in overall cardiovascular physiology.
Kidney’s Involvement in Sodium Handling
The kidneys play a crucial role in regulating blood pressure through the management of sodium levels. Renal artery perfusion pressure directly influences sodium excretion, a process known as pressure natriuresis. This affects vasoactive systems like the renin-angiotensin-aldosterone system (PubMed).
In an average adult, the kidney filters approximately 20-25 moles of sodium per day. More than 99% of the filtered sodium is reabsorbed into the bloodstream via various sodium transporters and exchangers located along different segments of the nephron. These include NHE3, NKCC2, NCC, ENaC, and pendrin, all of which are controlled by the renin-angiotensin-aldosterone system.
| Nephron Segment | Primary Sodium Transporter/Exchanger |
|---|---|
| Proximal Tubule | NHE3 |
| Thick Ascending Limb | NKCC2 |
| Distal Convoluted Tubule | NCC |
| Collecting Duct | ENaC, Pendrin |
Furthermore, salt intake is a significant determinant of blood pressure. Reduced dietary salt intake can lower morbidity and mortality rates related to hypertension and cardiovascular events. The kidney modulates blood pressure through extracellular fluid volume regulation, acquired via salt reabsorption activity controlled by the renin-angiotensin-aldosterone system (Clinical Kidney Journal).
Animal models have also provided insights into the role of specific sodium transporters, such as NHE3, in maintaining blood pressure. For instance, global NHE3 deletion and other targeted mouse models demonstrated significant alterations in blood pressure, urine volume, and plasma hormone levels (Clinical Kidney Journal).
Monogenic Forms of Hypertension
Monogenic forms of hypertension are genetic conditions that prominently affect the kidney’s role in sodium handling and transport. These conditions underline the significance of renal function in overall blood pressure regulation.
In patients with monogenic hypertension, specific genetic mutations alter the function of proteins involved in sodium reabsorption. This impacts the kidney’s ability to handle sodium properly, leading to elevated blood pressure. Understanding these genetic forms of hypertension can help in developing targeted treatment strategies.
For those interested in exploring more about the cardiovascular system and its interconnections, check out our articles on heart function and blood flow dynamics, vascular system adaptation, and cardiac disease mechanisms.
Impact of Kidney Disorders on Blood Pressure
Secondary Forms of Hypertension
Disorders that affect the kidney or its blood vessels often result in secondary forms of hypertension. This condition arises due to the intricate connection between kidney function and blood pressure regulation. The renal-angiotensin-aldosterone system (RAAS) is a crucial mechanism involved in this interplay. The RAAS regulates blood pressure by enhancing sodium reabsorption, water retention, and increasing vascular tone. When RAAS is overly active, it can lead to elevated blood pressure, contributing to conditions such as renal artery stenosis and chronic kidney disease.
| Mechanism | Influence on Blood Pressure |
|---|---|
| Sodium Reabsorption | Increases |
| Water Retention | Increases |
| Vascular Tone | Increases |
Additionally, secondary hypertension can arise due to conditions like polycystic kidney disease or glomerulonephritis. These illnesses hinder the kidney’s ability to filter blood efficiently, leading to fluid buildup and heightened blood pressure. Understanding these secondary forms of hypertension is essential for comprehending the broader aspects of blood pressure regulation and cardiac disease mechanisms.
Experimental Models of Hypertension
Experimental models of hypertension provide vital insights into the relationship between kidney function and blood pressure. One such model is the Dahl salt-sensitive rat. Studies using this model have illustrated the effects of kidney transplantation on blood pressure regulation. Specifically, the blood pressure response to sodium intake mirrors the characteristics of the transplanted kidney.
By utilizing these models, researchers can elucidate the underlying mechanisms that lead to elevated blood pressure due to impaired kidney function. These findings are crucial for developing targeted interventions and therapies aimed at mitigating hypertension induced by renal disorders. To further explore how blood pressure regulation is affected by kidney disorders and other physiological processes, refer to our detailed analysis on vascular system adaptation.
Low Blood Pressure
Low blood pressure, also known as hypotension, is a condition that plays a significant role in blood pressure regulation. It can affect individuals of any age and background, and understanding its definition, prevalence, symptoms, and potential causes is crucial in the realm of cardiovascular physiology.
Definition and Prevalence
Low blood pressure is defined as a reading below 90/60 mm Hg, whereas normal blood pressure ranges from 90/60 mm Hg to 120/80 mm Hg (Cleveland Clinic).
| Category | Systolic (mm Hg) | Diastolic (mm Hg) |
|---|---|---|
| Normal Blood Pressure | 90 – 120 | 60 – 80 |
| Low Blood Pressure | < 90 | < 60 |
The prevalence of low blood pressure varies widely. While it can be a benign condition for some, in others, it may indicate underlying health issues requiring medical attention.
Symptoms and Potential Causes
Symptoms of low blood pressure often arise when certain body parts do not receive adequate blood flow due to rapid decreases in blood pressure. Some common symptoms include:
- Dizziness
- Fainting
- Blurred vision
- Nausea
- Fatigue
These symptoms can be unpleasant and disruptive, and in severe cases, dangerous.
Potential causes of low blood pressure include:
- Dehydration: Reduced blood volume can lead to decreased pressure.
- Heart Problems: Conditions like bradycardia or heart failure can lower blood pressure. Learn more about this in our section on heart function and blood flow dynamics.
- Endocrine Issues: Disorders such as adrenal insufficiency can impact blood pressure regulation.
- Medications: Certain drugs can cause hypotension as a side effect. Dosage adjustments or discontinuation might be necessary.
- Blood Loss: Severe injuries or surgeries causing blood loss can reduce pressure.
- Septicemia: Severe infections can result in septic shock, significantly dropping blood pressure.
In treating low blood pressure, addressing the underlying cause is essential. This may range from simple interventions like IV fluids to more complex solutions such as surgery or even heart transplants in severe cases. For more information on cardiac-related conditions, visit our section on cardiac disease mechanisms.
Understanding the various aspects of low blood pressure is key to managing and preventing it effectively. For additional information on how the body adapts to varying blood pressures, see our section on vascular system adaptation.
Baroreceptors in Blood Pressure Regulation
Baroreceptors play a pivotal role in maintaining systemic blood pressure and ensuring stable cardiovascular function. Understanding their function and significance offers insight into the intricate mechanisms of blood pressure regulation.
Role of Baroreceptors in Maintaining Blood Pressure
Baroreceptors are specialized sensors located in the cardiovascular system that detect changes in blood pressure. They play a critical role in the body’s ability to respond to acute demands by adjusting peripheral vascular resistance and cardiac output (NCBI Bookshelf). These sensors are primarily responsible for preventing rapid fluctuations in blood pressure and maintaining a relatively constant level, even during activities such as standing up or lying down (Boundless).
| Function | Mechanism |
|---|---|
| Detection | React to stretching of arterial walls due to blood pressure changes |
| Response | Adjust nerve signals to dilate or constrict blood vessels |
| Regulation | Influence heart rate and force of contractions |
Their main function involves detecting the stretch in the arterial walls caused by changes in blood pressure. When blood pressure rises, baroreceptors increase their firing rate, sending signals to the brain to decrease heart rate and dilate blood vessels, thereby lowering blood pressure. Conversely, when blood pressure drops, they reduce their firing rate, prompting an increase in heart rate and vasoconstriction (Physio-Pedia).
High and Low Pressure Baroreceptors
Baroreceptors are categorized into high pressure and low pressure types, each playing distinct roles in blood pressure regulation.
High Pressure Baroreceptors (Arterial Baroreceptors):
High pressure baroreceptors are located in the carotid sinuses and aortic arch. These receptors are crucial for minute-to-minute regulation of arterial pressure. They respond to the stretch from elevated blood pressure by signaling the central nervous system to induce vasodilation and decrease cardiac output.
- Location: Carotid sinuses, Aortic arch
- Role: Immediate regulation of arterial pressure
- Response: Modulate heart rate and vascular tone
Low Pressure Baroreceptors (Cardiopulmonary Baroreceptors):
Low pressure baroreceptors are found in the walls of the atria, ventricles, and pulmonary arteries. They primarily monitor blood volume rather than pressure. These receptors help regulate hormone secretion, salt and water retention, and overall blood volume by influencing the kidneys and other organs.
- Location: Atria, Ventricles, Pulmonary arteries
- Role: Regulation of blood volume and fluid balance
- Response: Influence hormone release and kidney function
The coordinated efforts of high and low pressure baroreceptors ensure that blood pressure remains within a narrow, healthy range, protecting the body from the adverse effects of hypertension and hypotension. For more insights into related mechanisms, explore articles on vascular system adaptation and cardiac disease mechanisms.
By grasping how baroreceptors function, health enthusiasts can better understand the delicate balance of the cardiovascular system and appreciate the body’s natural regulatory mechanisms.
High Blood Pressure Consequences
High blood pressure, or hypertension, can lead to a multitude of adverse effects on the body. It’s important to understand how it can specifically impact the arteries and vital organs.
Damage to Arteries
High blood pressure increases the pressure of blood flowing through the arteries. Over time, this can cause significant damage to the arterial walls. The persistent high pressure can lead to the following complications:
- Arterial Stiffening: High blood pressure makes arteries less flexible, which can make it harder for blood to flow efficiently.
- Aneurysms: Weak spots in arteries can bulge and form aneurysms, which pose a risk of rupture.
- Narrowing of Arteries: Plaque buildup (atherosclerosis) can be accelerated, leading to narrowed arteries and reduced blood flow.
The damage to arterial walls can have severe consequences on organs and tissues that depend on the smooth flow of blood for nutrients and oxygen (Mayo Clinic). The structural integrity and function of the arteries are critical in maintaining overall cardiovascular health.
Effects on Vital Organs
Hypertension can affect various vital organs including the heart, brain, and kidneys, leading to a host of complications.
-
Heart:
- Heart Disease: High blood pressure puts additional strain on the heart, which can lead to heart disease, including hypertrophy (thickening of the heart muscle), heart failure, and coronary artery disease.
- Heart Attack: Increased arterial damage and reduced blood flow can result in a heart attack.
-
Brain:
- Stroke: High blood pressure can cause blood vessels in the brain to burst or become blocked, leading to a stroke.
- Cognitive Decline: It can also affect memory and cognitive function over time due to reduced blood flow to brain tissues.
-
Kidneys:
- Kidney Damage: Hypertension can damage the blood vessels in the kidneys, leading to impaired kidney function. This is particularly exacerbated in individuals with diabetes (Mayo Clinic).
- Kidney Failure: Prolonged high blood pressure can lead to kidney failure, necessitating dialysis or a kidney transplant.
| Organ | High Blood Pressure Effects |
|---|---|
| Arteries | Stiffening, Aneurysms, Atherosclerosis |
| Heart | Heart Disease, Heart Attack, Hypertrophy |
| Brain | Stroke, Cognitive Decline, Memory Issues |
| Kidneys | Kidney Damage, Kidney Failure |
For more in-depth information on the physiological effects of high blood pressure on the heart and vascular system, explore our articles on heart function and blood flow dynamics and vascular system adaptation. Additionally, understanding cardiac disease mechanisms can provide insights into the broader implications of hypertension on cardiovascular health.
- About the Author
- Latest Posts
Johnnie D. Jackow Sr., the founder and CEO of Total Body Fitness, Worldwide, has a long-standing career in the fitness industry. He began as a certified personal trainer in the mid-90s and soon after authored his first weight loss book in 1998. This led to the launch of Total Body Fitness, Nationwide in the USA at the same time. Johnnie gained recognition as the fitness guru of his time, running infomercials on local TV late at night in Houston, Texas. Over the years, he has helped more than 40,000 individuals from all over the world achieve their health and fitness goals. With over 60,000 hours of documented training in integrative functional medicine, he completed his PhD in human physiology in 2010. His primary objective is to assist people in reaching their health and fitness goals through alternative approaches rather than relying solely on conventional medicine and pharmaceutical drugs. Today, with almost three decades of experience under his belt, Johnnie continues to be a leader in health and fitness.