The Basics of Cardio Physiology
Understanding the cardiovascular system is vital for grasping how various forms of exercise impact overall health. This section delves into the essentials of how the vascular system operates and the profound impact that regular physical activity has on it.
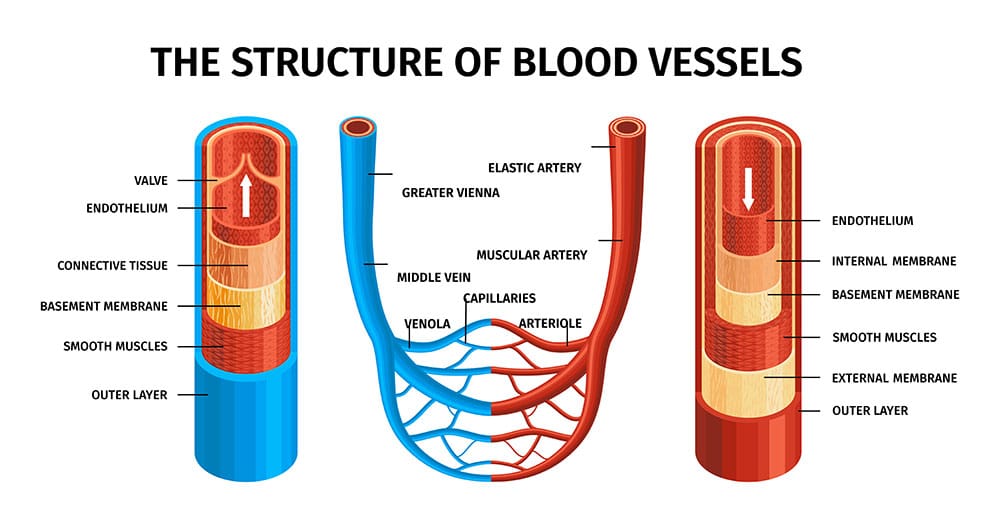
Understanding the Vascular System
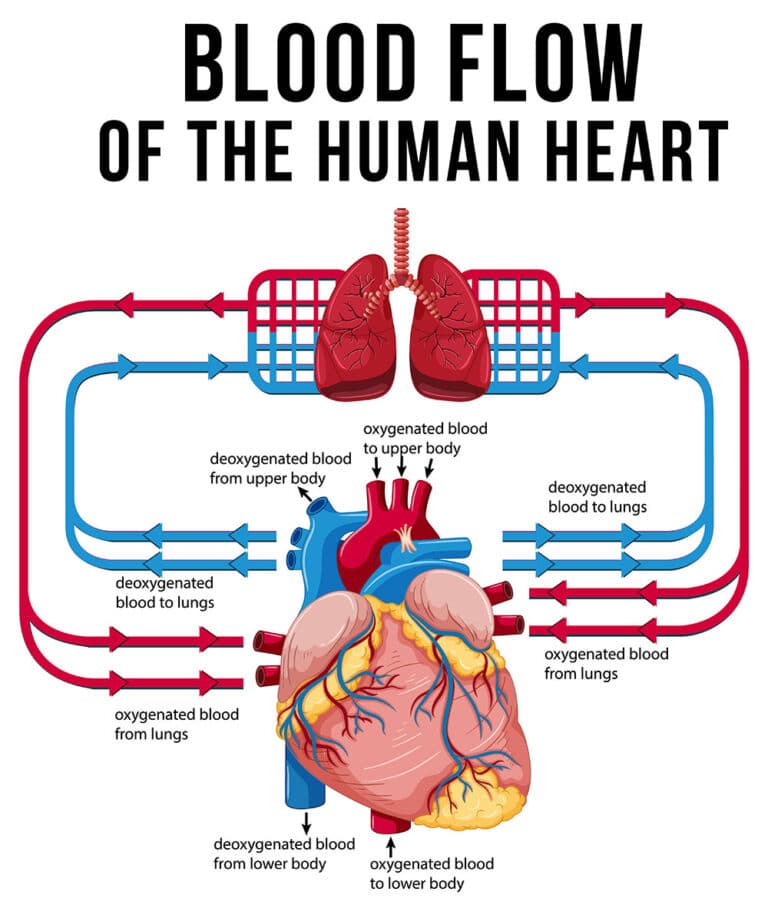
The vascular system, consisting of arteries, veins, and capillaries, plays a crucial role in transporting blood throughout the body. It is divided into two primary circuits: the systemic and pulmonary circuits. The systemic circuit delivers oxygenated blood from the heart to various body tissues, while the pulmonary circuit transports deoxygenated blood from the heart to the lungs for oxygenation.
| Component | Function |
|---|---|
| Arteries | Carry oxygenated blood away from the heart |
| Veins | Carry deoxygenated blood back to the heart |
| Capillaries | Facilitate the exchange of oxygen, carbon dioxide, and nutrients |
A healthy vascular system ensures efficient blood flow, regulates blood pressure, and maintains overall homeostasis. It adapts to various stimuli, including physical exercise, by making structural and functional changes that improve cardiovascular efficiency. For a more detailed look at blood flow dynamics, visit heart function and blood flow dynamics.
Impact of Regular Physical Exercise
Regular physical activity brings numerous benefits, particularly in the context of cardiovascular health. Exercise training improves oxygen delivery, enhances substrate metabolism, and increases mitochondrial mass (NCBI). It also positively influences factors like muscle-ECM-tendon unit stiffness and neural adaptation. These adaptations contribute to improved running and cycling economy, enhanced muscle recruitment patterns, increased muscle coactivation, and more efficient muscle activity.
| Exercise Adaptation | Benefit |
|---|---|
| Improved Oxygen Delivery | Enhanced endurance and performance |
| Increased Mitochondrial Mass | Better energy production and utilization |
| Neural Adaptation | Optimized muscle recruitment and coordination |
Exercise has been shown to reduce blood pressure in hypertensive individuals, highlighting its importance in managing and preventing hypertension (Physio-Pedia). Additionally, physical activity reduces the risk of primary and secondary cardiovascular events like myocardial infarction and stroke. It also helps manage chronic diseases with vascular origins, such as diabetes and dementia, via changes in cardiovascular risk factors and direct effects on arterial shear stress and mechanotransduction.
Regular exercise induces beneficial effects on heart function. Adaptations include a lower resting heart rate and cardiac hypertrophy, which are linked to a variety of changes in tissue metabolism and signaling (Frontiers in Cardiovascular Medicine). Furthermore, physical activity increases vasodilation and the availability of vasodilatory mediators like nitric oxide, which suppresses atherogenesis and enhances vascular function (Frontiers in Cardiovascular Medicine).
For more information on the mechanisms underlying cardiovascular diseases, visit our article on cardiac disease mechanisms. To understand how regular activity aids in maintaining optimal blood pressure, see blood pressure regulation.
Cardiovascular Adaptations to Exercise
Physical exercise has profound effects on the cardiovascular system, leading to various adaptations that enhance overall health and performance. Here we explore the vascular changes that come with exercise training and the effects of exercise on inflammation.
Vascular Changes with Exercise Training
Exercise training results in several adaptations within the vascular system. One of the primary adaptations is an increase in capillary density in skeletal muscles, which enhances the delivery of oxygen and nutrients to the muscles during physical activity. This, in turn, increases exercise capacity and performance.
The changes and measurements include:
- Increased capillary density
- Improved arterial flexibility
- Enhanced endothelial function
| Vascular Adaptation | Impact |
|---|---|
| Capillary Density | Increased oxygen and nutrient delivery to muscles |
| Arterial Flexibility | Reduced risk of atherosclerosis |
| Endothelial Function | Improved blood flow and reduced vascular resistance |
Moreover, long-term dynamic aerobic training has been shown to reduce blood pressure, which positively impacts cardiovascular health. This reduces the risk of cardiovascular diseases like hypertension and stroke.
Effects of Exercise on Inflammation
Regular physical activity has a notable anti-inflammatory effect. Exercise reduces chronic inflammation associated with obesity, type 2 diabetes, and cardiovascular disease. This anti-inflammatory response helps protect against the development of atherosclerosis (PMC).
Inflammatory Markers:
- C-Reactive Protein (CRP)
- Tumor Necrosis Factor-alpha (TNF-α)
- Interleukin-6 (IL-6)
Exercise impacts the development of atherosclerosis and the occurrence of cardiovascular events by ameliorating chronic diseases with a vascular etiology. This is achieved through primary mechanisms, such as improving endothelial function, and secondary mechanisms, like reducing inflammatory markers. For detailed insights into heart function and blood flow dynamics, read more on our site.
| Inflammatory Marker | Effect of Exercise |
|---|---|
| CRP | Decreased levels |
| TNF-α | Reduced levels |
| IL-6 | Balanced levels |
Understanding these adaptations can help individuals optimize their exercise routines to maximize cardiovascular health. Regular exercise, therefore, plays a crucial role in mitigating the risks associated with chronic diseases and improving vascular system functionality. For more on how exercise affects blood pressure regulation and cardiac disease mechanisms, visit the relevant sections.
Mechanisms of Cardio Adaptation
Mitochondrial Biogenesis in the Heart
Mitochondrial biogenesis, the process by which new mitochondria are formed in the cell, is a critical mechanism in the cardiovascular adaptation to exercise. Regular physical activity stimulates this process in cardiomyocytes, the cells of the heart muscle, contributing significantly to vascular system adaptation. Enhanced mitochondrial biogenesis leads to an increase in oxidative capacity, allowing the heart to produce more energy efficiently and remain resilient against conditions such as ischemia-reperfusion injury (PMC).
Key benefits of mitochondrial biogenesis in the heart include:
- Improved energy production: Increased oxidative capacity allows for better ATP synthesis.
- Enhanced protection: Mitochondria help protect against ischemic damage and support recovery after injury.
- More efficient heart function: Better energy management supports improved systolic and diastolic function.
Role of Myokines in Cardio Health
Myokines are cytokines released by skeletal muscles during exercise that play a vital role in the interplay between muscle and cardiovascular health. These molecules facilitate inter-tissue crosstalk, mediating various systemic health benefits. For individuals aiming to understand the vascular system adaptation, it’s crucial to recognize how myokines influence cardiovascular physiology.
The primary effects of myokines on cardiovascular health include:
- Reducing inflammation: Myokines combat systemic inflammation, lowering the risk of chronic cardiovascular diseases.
- Enhancing metabolism: They boost fatty acid oxidation and glucose uptake, improving overall metabolic efficiency.
- Improving insulin sensitivity: They play a role in increasing insulin secretion and sensitivity, benefiting heart health (PMC).
Understanding these mechanisms highlights the importance of regular physical exercise in maintaining a healthy cardiovascular system. It also underscores how molecular adaptations drive the improvements seen in heart function and blood flow dynamics.
To visualize the key impacts of myokines on cardio health, consider the following table:
| Myokine Function | Impact on Cardiovascular Health |
|---|---|
| Reducing Inflammation | Lowers chronic disease risk |
| Enhancing Fatty Acid Oxidation | Improves metabolic health |
| Increasing Glucose Uptake | Supports energy balance |
| Enhancing Insulin Sensitivity | Protects against diabetes |
For ongoing learning about the mechanisms of cardio adaptation, refer to our articles on blood pressure regulation and cardiac disease mechanisms. Understanding these insights can empower health enthusiasts to optimize their exercise routines for maximum cardiovascular benefit.
Gender Differences in Cardiovascular Function
Aging Women vs. Aging Men
Cardiovascular function exhibits significant differences between aging men and women. Studies have shown that older women experience greater declines in both cardiac and autonomic cardiovascular function. These declines include reduced left ventricular relaxation and increased muscle sympathetic nerve activity, which contribute to a higher incidence of cardiovascular morbidity and mortality in postmenopausal women.
Key differences include:
- Left Ventricular Relaxation: Older women exhibit reduced relaxation compared to men.
- Sympathetic Nerve Activity: Increased activity in older women contributes to greater cardiovascular stress.
| Cardiovascular Function | Aging Women | Aging Men |
|---|---|---|
| Left Ventricular Relaxation | Reduced | Less reduced |
| Sympathetic Nerve Activity | Increased | Less increased |
| Cardiovascular Morbidity | Higher | Lower |
Impacts on Cardiac Output
Cardiac output, the amount of blood the heart pumps per minute, is another area where gender differences are evident. There is a steeper decline in maximal cardiac output in older men (age 60-90) compared to older women. Despite this, men show greater reductions in left ventricular mass and maximal cardiac power output. In contrast, women tend to preserve these measures as they age (NCBI).
Key findings:
- Maximal Cardiac Output: Decreases more steeply in older men.
- Left Ventricular Mass: Declines in men but remains stable in women.
- Maximal Cardiac Power Output: Lower in aging men compared to women.
| Cardiovascular Measure | Aging Women | Aging Men |
|---|---|---|
| Maximal Cardiac Output | Less steep decline | Steeper decline |
| Left Ventricular Mass | Stable | Declines |
| Maximal Cardiac Power | Stable | Declines |
Additionally, the relationship between the heart’s pumping capacity and peripheral vascular reserve changes with age, displaying more pronounced sex differences. Specifically, leg vasodilator reserve and systemic aerobic capacity show a stronger correlation in older men compared to women (NCBI).
- Peripheral Vascular Reserve: Stronger association with systemic capacity in men.
- Systemic Aerobic Capacity: More pronounced sex differences noted with age.
| Measure | Aging Women | Aging Men |
|---|---|---|
| Peripheral Vascular Reserve | Less associated | Stronger association |
| Systemic Aerobic Capacity | Less associated | Stronger association |
These gender-specific differences underline the complexity of heart function and blood flow dynamics as well as blood pressure regulation across different age groups. Tailored cardiovascular strategies might be essential for addressing these variations and improving overall heart health in aging populations. For more insights into cardiovascular mechanisms, visit our section on cardiac disease mechanisms.
Vascular Responses to Exercise
Understanding how exercise affects the vascular system is crucial for those aiming to improve cardiovascular health. Chronic physical activity and the intensity of exercise play significant roles in vascular function and adaptation.
Chronic Exercise and Vascular Function
Chronic physical activity profoundly impacts vascular function. Repeated bouts of exercise result in both functional adaptations and structural remodeling of arteries. One of the most notable changes is the enhanced ability of blood vessels to dilate, a process facilitated by the increased availability of vasodilatory mediators such as nitric oxide.
Regular physical activity boosts the production and bioavailability of nitric oxide, which helps to suppress the development of atherosclerosis. Additionally, chronic exercise leads to an increase in vascular density and the capacity for vasodilation, which, in turn, enhances the perfusion of blood through skeletal muscle.
| Measurement | Before Exercise Training | After Exercise Training |
|---|---|---|
| Nitric Oxide Levels | Baseline | Increased |
| Vascular Density | Normal | Increased |
| Vasodilatory Capacity | Standard | Enhanced |
These adaptations promote better overall cardiovascular health and reduce the risk of cardiac disease.
Impact of Exercise Intensity
The intensity of exercise also plays a crucial role in inducing vascular adaptations. During acute exercise, small arteries and pre-capillary arterioles must dilate to accommodate the increased blood flow needed by working muscles. This dilation is driven by vasodilatory signals such as adenosine, lactate, potassium, hydrogen ions, and carbon dioxide (Frontiers in Cardiovascular Medicine).
Higher-intensity exercise sessions result in more pronounced vascular responses and greater adaptive changes over time. These include increased blood flow dynamics and more efficient delivery of oxygen and nutrients to tissues, enhancing heart function and blood flow dynamics.
Exercise intensity also affects the production of endothelium-derived substances, critical for antiatherogenic effects. As endothelial cells possess significant plasticity, they adapt to both intrinsic genetic factors and extrinsic environmental influences, thus contributing to the overall adaptation and improved vascular function (NCBI Bookshelf).
For those seeking to optimize their cardiovascular health, understanding these vascular responses and adjusting exercise intensity can be critical in maximizing benefits. For further reading on how exercise affects blood pressure, check out our article on blood pressure regulation.
Genetic Influences on Training
Understanding individual responses to exercise and the role genetics play is fundamental to unraveling the complexities of the vascular system adaptation.
Individual Responses to Exercise
The way individuals respond to exercise can vary significantly. These variations are attributed to several factors, including genetic makeup, which plays a significant role in how one’s cardiovascular system adapts to physical training. Not everyone will experience the same improvements in heart function, blood flow dynamics, or blood pressure regulation after engaging in an exercise regimen.
For example, studies suggest that individuals with a specific genetic profile may exhibit greater enhancements in heart rate variability and a more significant reduction in blood pressure compared to others. This variability emphasizes the need to personalize exercise programs to maximize cardiovascular benefits.
Role of Genetics in Training Adaptations
Genetics influence several aspects of cardiovascular adaptations triggered by exercise. Key genetic factors include:
- Gene Variants: Certain gene variants are associated with increased aerobic capacity, improved mitochondrial function, and enhanced muscle efficiency.
- Heritability: Approximately 50% of the variability in exercise adaptation can be attributed to heritability. This means that genetic factors significantly impact how the vascular system responds to exercise.
| Genetic Factor | Impact on Training Adaptation |
|---|---|
| ACE Gene | Associated with endurance and cardiovascular efficiency |
| ACTN3 Gene | Linked to muscle performance and power output |
| PGC-1α Gene | Influences mitochondrial biogenesis and oxidative capacity |
Understanding these genetic influences can help develop more effective and personalized training programs. This tailored approach can lead to better cardiovascular outcomes, including reduced resting heart rate, improved lipid profiles, and enhanced vascularization (PMC).
Internal links such as blood pressure regulation and heart function and blood flow dynamics provide further insights into how genetics and training adaptations interact to affect overall cardiovascular health.
- About the Author
- Latest Posts
Johnnie D. Jackow Sr., the founder and CEO of Total Body Fitness, Worldwide, has a long-standing career in the fitness industry. He began as a certified personal trainer in the mid-90s and soon after authored his first weight loss book in 1998. This led to the launch of Total Body Fitness, Nationwide in the USA at the same time. Johnnie gained recognition as the fitness guru of his time, running infomercials on local TV late at night in Houston, Texas. Over the years, he has helped more than 40,000 individuals from all over the world achieve their health and fitness goals. With over 60,000 hours of documented training in integrative functional medicine, he completed his PhD in human physiology in 2010. His primary objective is to assist people in reaching their health and fitness goals through alternative approaches rather than relying solely on conventional medicine and pharmaceutical drugs. Today, with almost three decades of experience under his belt, Johnnie continues to be a leader in health and fitness.